Ann Oncol: 肿瘤患者营养支持可降低死亡率:一项前瞻性随机研究的二次分析结果
2021-07-19 yd2015 MedSci原创
研究表明,肿瘤患者加强营养支持质量可将死死亡风险以及改善功能和生活质量。
williamhill asia 知道,肿瘤患者的营养支持治疗目的多为改善患者的生活质量。但是其对于患者的预后的作用不明确。因此,来自国外的研究团队对一项前瞻性随机研究的进行二次分析,旨在比较营养支持(干预组)对比对照组对于30天死亡率的影响。相关研究结果发表在Annals of Oncology杂志上。
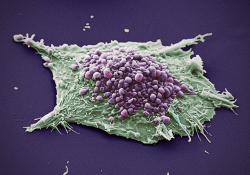
该研究(EFFORT)是瑞士前瞻性、随机对照的多中心研究。纳入506例患者,其中营养支持干预组为255例,对照组为251例。常见的肿瘤类型为肺癌(113例),血液肿瘤(108例),胃肠道肿瘤(84例)以及其他肿瘤(201例)。
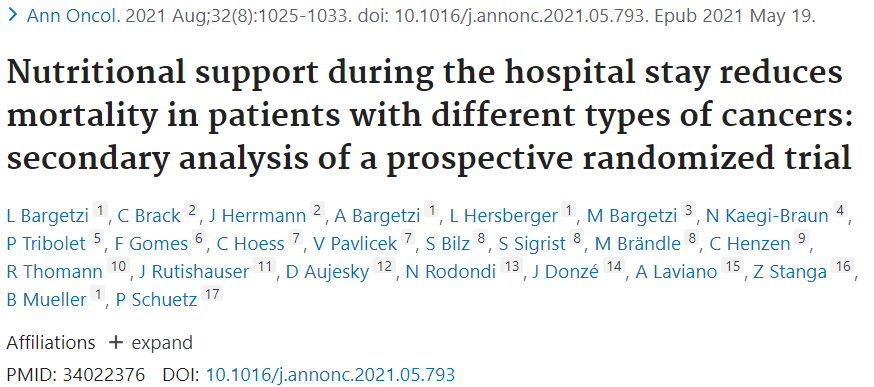
基于营养风险筛查(NRS 2002)的NRS评分是180天死亡的独立预测因素,校正的HR为1.29 (95% CI 1.09-1.54; P=0.004,每增加NRS一分)。随着NRS的升高,患者的生存越短。也可观察到随着NRS越高与不利预后的关系(OR=1.42 (95% CI 1.11-1.83); P =0.006])。同时也类似观察到其对中位住院时间、功能下降和生活质量的影响。
NRS对死亡影响
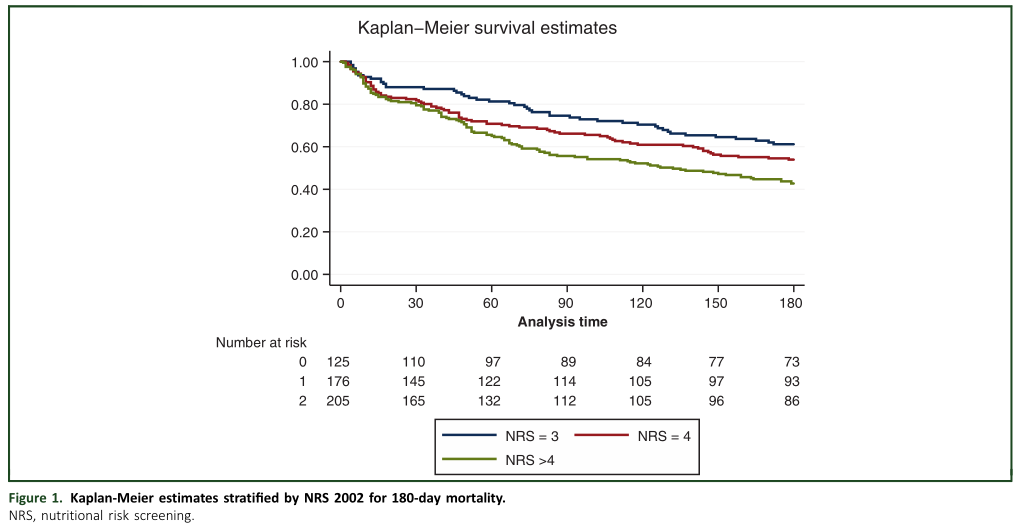
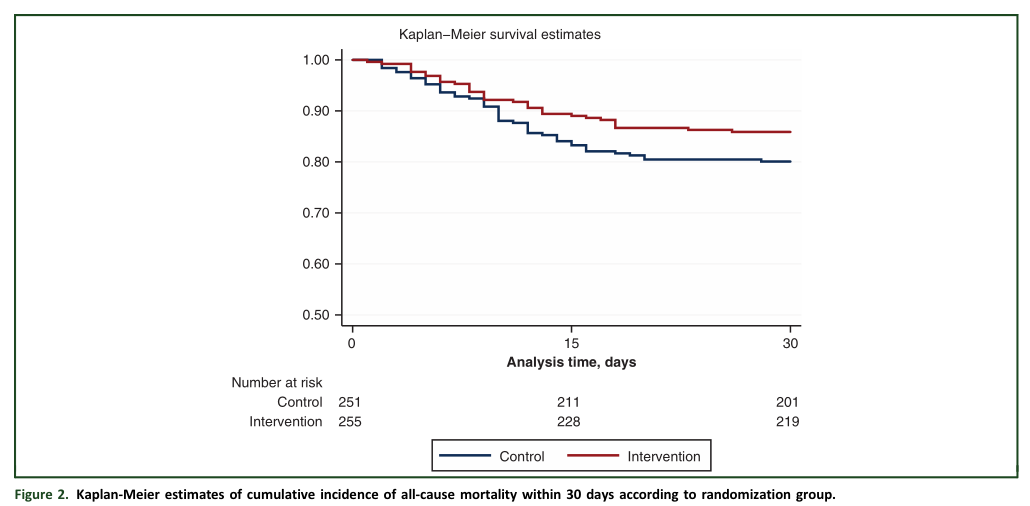
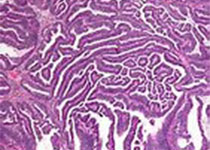
30天随访期间,对照组中有50例(19.9%)患者死亡,而干预组中有36例 (14.1%)患者死亡,校正的OR为0.57 (95% CI 0.35-0.94; P= 0.027)。大于6个月的随访,对照组中有128例(52.7%)患者死亡,而干预组中有115例 (47.3%)患者死亡,校正的OR为0.83 (95% CI 0.65-1.08, P =0.18)。
30天死亡分析
两组对生存影响
与营养支持干预组相比,对照组日常生活功能下降更明显[校正OR=0.59 (95% CI 0.38-0.93); P =0.021]。同时,营养支持干预组明显改善患者的生活质量,通过EQ-5D指数评估时 [校正系数 =0.08 (95% CI 0.01-0.15); P=0.016] 和通过EQ-5D VAS评估时 [校正系数=6.16 (95% CI 0.51-11.8); P =0.033]。
进行亚组分析时,发现两组的30天死亡比较没有明显差异。

亚组分析
综上,研究表明,肿瘤患者加强营养支持质量可将死死亡风险以及改善功能和生活质量。
原始出处:
Bargetzi L, Brack C, Herrmann J, et al. Nutritional support during the hospital stay reduces mortality in patients with different types of cancers: secondary analysis of a prospective randomized trial. Ann Oncol. 2021 Aug;32(8):1025-1033. doi: 10.1016/j.annonc.2021.05.793. Epub 2021 May 19. PMID: 34022376.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#前瞻性#
57
#Oncol#
52
学习了
58
#随机研究#
62
#营养支持#
58
#肿瘤患者#
57
谢谢williamhill asia 分享这么多精彩信息
78
高质量研究,读起来真爽,谢谢williamhill asia
77