罗氏将启动阿尔茨海默病药物 gantenerumab 的新 III 期研究
2022-02-27 Allan MedSci原创
在SCarlet RoAD和Marguerite RoAD开放标签扩展研究中,gantenerumab显著降低了散发性阿尔茨海默病患者的淀粉样蛋白斑块。
近日,罗氏计划开始一项新的 III 期试验(SKYLINE 研究),评估其抗淀粉样蛋白β抗体 gantenerumab 在阿尔茨海默病早期阶段的受试者中的有效性和安全性。这项新研究计划于 6 月开始。
根据 ClinicalTrials.gov 的数据,SKYLINE 研究预计将招募 1200 例淀粉样蛋白阳性、认知功能未受损的参与者,这些参与者有患阿尔茨海默病的风险或处于阿尔茨海默病的早期阶段。受试者将随机接受皮下注射 gantenerumab 或安慰剂,主要终点是评估临床前阿尔茨海默氏症认知复合 5 (PACC-5) 评分从基线到第四年的变化。
罗氏曾表示,在 SCarlet RoAD 和 Marguerite RoAD 开放标签扩展研究中,gantenerumab 显著降低了散发性阿尔茨海默病患者的淀粉样蛋白斑块;在DIAN-TU-001 研究中,gantenerumab 减少率显性遗传的阿尔茨海默病患者的淀粉样蛋白斑块。然而,所有三个试验最终都没有成功。
阿尔茨海默病(老年痴呆)是一种发病进程缓慢、随着时间不断恶化的神经退化性疾病,此病症占了痴呆症中六到七成的成因。最常见的早期症状为丧失短期记忆(难以记住最近发生的事),当疾病逐渐进展,症状可能逐渐出现,包括语言障碍、定向障碍(包括容易迷路)、情绪不稳、丧失动机、无法自理和许多行为问题。疾病的进程与大脑中的纤维状类淀粉蛋白质斑块沉积和Tau蛋白有关。
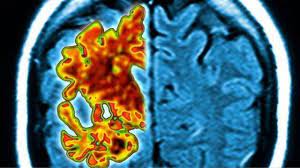
1991年,学者提出类淀粉胜肽假说,认为β类淀粉胜肽(Aβ)在大脑堆积可能是导致阿尔茨海默病的根本原因。进一步的证据则是来自于基因克隆鼠实验,研究人员在实验鼠身上表现突变型人类APP基因,结果发现其大脑会产生纤维状类淀粉蛋白斑块,并出现类似阿尔茨海默病的大脑病理变化及空间学习障碍。
原始出处:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#III#
71
#阿尔茨海#
64
#阿尔茨#
62
#mAb#
73
#阿尔茨海默#
61