Crit Care:抗血小板治疗能预防急性呼吸窘迫综合征吗?
2018-03-12 xing.T MedSci原创
由此可见,抗血小板治疗并没有显著降低高危患者的住院死亡率。然而,抗血小板治疗是否能降低ARDS高风险患者发生这种疾病的发生率尚不清楚。
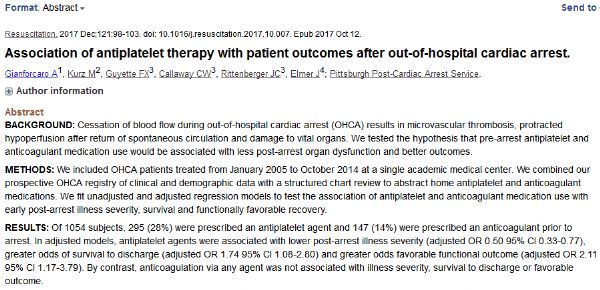
急性呼吸窘迫综合征(ARDS)是一种危及生命的疾病,死亡率高,造成严重的医疗负担。抗血小板治疗是一种潜在的治疗策略,以防止高ARDS风险的个体发生这种疾病。近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,研究人员进行了一项荟萃分析研究抗血小板治疗能否降低高危患者新发ARDS的发生率及其相关死亡率。
研究人员采用Cochrane对照试验登记中心、PubMed、EMBASE、MEDLINE和Web of Science等数据库检索了数据库从成立到2017年10月26日期间发表的相关文献。研究人员纳入了调查医院或重症监护病房接受抗血小板治疗的ARDS高位患者的随机临床试验、队列研究和病例对照研究。研究人员提取了基线患者特征、干预、对照和结局。该研究的主要结局是高危患者新发ARDS的发生率。次要结局是医院和ICU死亡率。研究人员采用随机效应或固定效应模型进行定量合成。
研究人员确定了九项符合条件的研究,包含了7660名接受抗血小板治疗的高危患者。根据七项观察性研究,抗血小板治疗与ARDS发生率降低(比值比(OR)为0.68,95%可信区间(CI)为0.52-0.88,I2=68.4%,P=0.004)相关。在两项随机研究中,抗血小板组和安慰剂组新发ARDS之间无显著性差异(OR为1.32,95%CI为0.72-2.42;I=0%,P=0.329)。在随机研究(OR为1.15,95%CI为0.58-2.27;I2=0%;P=0.440)或观察性研究(OR为0.80,95%CI为0.62-1.03;I2=31.9%,P=0.221)中,抗血小板治疗并没有降低住院死亡率。
由此可见,抗血小板治疗并没有显著降低高危患者的住院死亡率。然而,抗血小板治疗是否能降低ARDS高风险患者发生这种疾病的发生率尚不清楚。
原始出处:
Yingqin Wang.et al. The preventive effect of antiplatelet therapy in acute respiratory distress syndrome: a meta-analysis.Critical Care.2018. https://doi.org/10.1186/s13054-018-1988-y
本文系williamhill asia
医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#综合征#
35
#呼吸窘迫#
36
学习了
63
了解一下.谢谢分享!
59