Blood:brentuximab vedotin联合达卡巴嗪或苯达莫司汀用于HL老年患者的安全性和治疗效果。
2017-10-17 qinqiyun MedSci原创
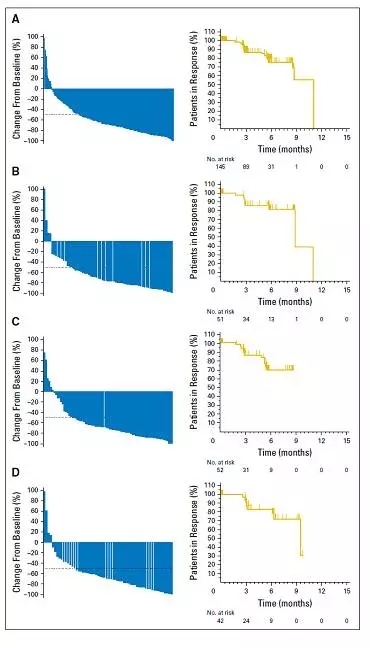
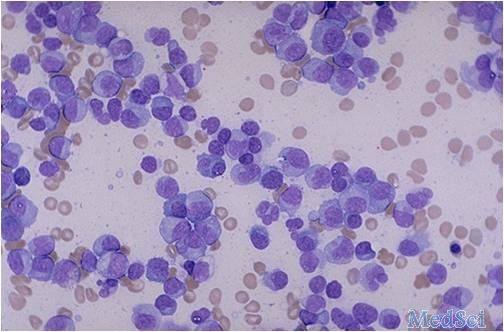
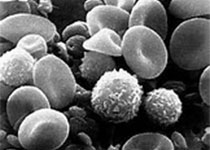
首次接受治疗的60岁及以上的霍奇金淋巴瘤(HL)患者,由于治疗相关的毒性作用和并发症,可选择的治疗方式很少,而且预后较差。现研究人员进行一非盲、非随机的II期研究,评估brentuximab vedotin(BV)单一疗法、BV+达卡巴嗪(DTIC)和BV+苯达莫司汀用于霍奇金淋巴瘤老年患者的耐受性、疗效和反应持续时间。
中心点:60岁及以上的HL患者对于BV+DTIC联合治疗方案具有良好的耐受性。虽然BV+苯达莫司汀的治疗效果较高,但HL老年患者不能耐受其毒副作用。摘要:首次接受治疗的60岁及以上的霍奇金淋巴瘤(HL)患者,由于治疗相关的毒性作用和并发症,可选择的治疗方式很少,而且预后较差。现研究人员进行一非盲、非随机的II期研究,评估brentuximab vedotin(BV)单一疗法、BV+达卡巴嗪(DTIC)和BV+苯达莫司汀用于霍奇金淋巴瘤老年患者的耐受性、疗效和反应持续时间。招募未进行过化疗的典型HL患者。22位患者接受12个疗程的1.8mg/kg BV+375mg/m2 DTIC;然后20位再接受6个疗程的1.8mg/kg BV+90/70mg/m2 苯达莫司汀。随后进行BV单一治疗。20位接受BV+苯达莫司汀治疗的患者中有65%的患者出现严重副反应事件,并有2例死亡,导致终止使用苯达莫司汀,以及停止招募。大部分患者的病程处于III/IV期,超过一半的患者有3种及以上的并发症或者至少存在某一方面的严重影响生活质量的损伤。接受BV+DTIC治疗的患者,客观反应率(ORR)100%,完全缓解
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#mAb#
44
#治疗效果#
49
#达卡巴嗪#
55
#Brentuximab#
55
#vedotin#
52
#苯达莫司汀#
60
谢谢分享
85
还不错哦
79