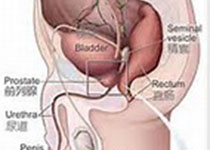
Sci Rep:骨钙素在患有勃起功能障碍的中年男性中的潜在保护性作用研究
2018-05-09 AlexYang MedSci原创
与勃起功能障碍(ED)相似,骨钙素(OC)同样被认为与心血管疾病(CVD)相关;然而,OC在ED中的作用仍旧不清楚。最近,有研究人员基于2009年9月到12月之间的防城港地区的男性健康调查(FAMHES)计划数据进行了相关的研究。研究人员利用国际勃起功能指数(IIEF-5)评估了ED情况。研究发现,OC与轻度(未调整: OR=0.647; P=0.016)或者中度(未调整:OR=0.453; P=
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#勃起#
46
#功能障碍#
45
#勃起功能#
51
学习了.谢谢分享
86