Mov Disord:服用磷酸甘油酸激酶1激活剂,与帕金森病的发病率有何关系?
2021-08-08 Freeman MedSci原创
增加对磷酸甘油酯激酶1激活剂和坦索罗辛的接触,都与PD发病率的小幅降低有关。这些结果支持进一步探究磷酸甘油酸酯激酶1激活剂和坦索罗辛改善PD的可能性。
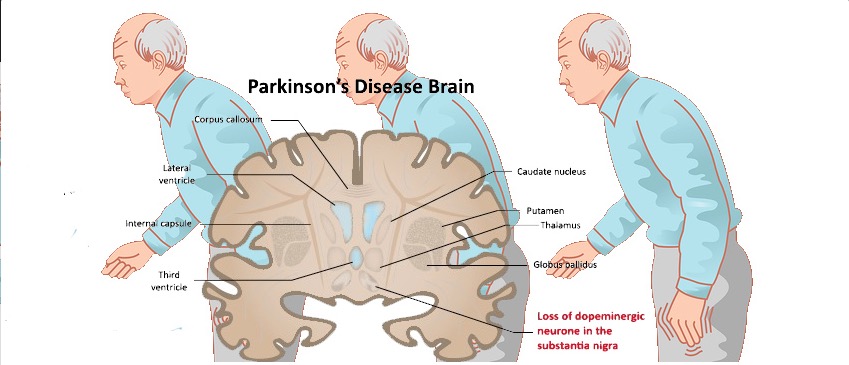
迄今为止,帕金森病(PD)尚无改变病情的治疗方法。
PD与葡萄糖和能量代谢受损有关,包括线粒体功能和氧化应激途径的异常。
有研究提出假设 :改善糖酵解可能对PD有益,Cai等人研究了特拉唑嗪(terazosin ),它通常用于治疗良性前列腺增生(BPH)的泌尿系统症状。
特拉唑嗪作为一种α1-肾上腺素(A1A)受体拮抗剂和磷酸甘油酸激酶1激活剂(PGK1a)。PGK1as激活一种在糖酵解过程中参与生成ATP的酶。
特拉唑嗪在PD的细胞和动物模型中具有神经保护特性。对人类队列的回顾性评估表明,与坦索罗辛(一种非PGK1a,也用于治疗前列腺增生症)相比,服用PGK1as的人结果更好。
藉此,加拿大多伦多大学的Priti Gros等人,在一个随访时间较长的大型队列中,试着验证这些结果。他们利用卫生健康数据库,探讨了接触PGK1as与PD发病率之间的关系。

具体来说:他们回顾性队列研究包括66岁以上新接触磷酸甘油酸激酶1激活剂或坦索罗辛的男性,并利用加拿大安大略省的卫生保健行政数据比较他们的PD发病率。
他们发现 :在265,745名男性中,累计使用磷酸甘油酸激酶1激活剂或坦索罗辛每增加一年,与PD发病率的危险性分别减少6%和8%。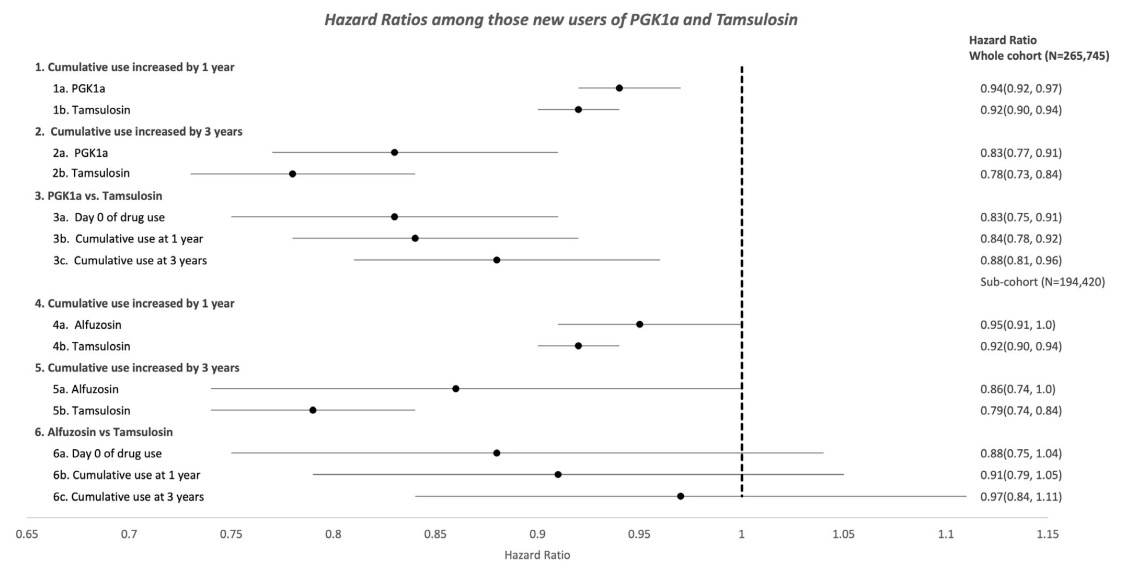
这些危害没有明显的差异(P = 0.2094)。
以6个月后和1、2年后为观察窗口的二级分析,也显示了类似的结果。
这个研究的重要意义在于发现了:增加对磷酸甘油酯激酶1激活剂和坦索罗辛的接触,都与PD发病率的小幅降低有关。这些结果支持进一步探究磷酸甘油酸酯激酶1激活剂和坦索罗辛改善PD的可能性。
原文出处:
Gros P, Wang X, Guan J, et al. Exposure to Phosphoglycerate Kinase 1 Activators and Incidence of Parkinson’s Disease. Mov Disord. Published online July 9, 2021:mds.28712. doi:10.1002/mds.28712
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言


















#发病率#
54
#Dis#
43
#Disord#
48
#激酶#
60