JGGD:头颈部基底细胞癌的皮镜手术对缩小切缘的研究
2022-06-23 医路坦克 MedSci原创
基底细胞癌(BCC)是最常见的皮肤癌本文的目的是评估皮镜检查是否可以有效地用于减少头颈部界限明确、无侵袭性基底细胞癌手术安全边界的宽度。
基底细胞癌(BCC)是最常见的皮肤癌,占所有皮肤恶性肿瘤的75 - 77%。其特点是生长缓慢,但具有浸润性和破坏性。紫外线照射区域是基底细胞癌的易发部位,尤其是浅肤色人群,约80%的病例发生在头颈部。特别是在面部,如果不治疗或不完全治疗,基底细胞癌可导致广泛的组织损伤。原发性基底细胞癌的治疗选择是完全手术切除并对切除边缘进行组织学检查。根据每一种基底细胞癌的复发风险,手术选择为金标准的三维(3D)显微切缘控制手术,或常规切缘宽5 - 15mm(高危基底细胞癌)和3 - 5mm(低风险基底细胞癌)的切除。德国最新的皮肤基底细胞癌S2k威廉亚洲博彩公司 建议,对于高复发风险基底细胞癌,常规切除>切缘5mm,包括头颈部H区(眼皮、眉毛、眶周、鼻子、上唇、颌角、耳前和耳后区、耳朵、鬓角)直径≥6mm的基底细胞癌和M区(脸颊、前额、下巴、下唇、头皮、颈部)直径≥10mm的基底细胞癌。
但在临床实践中,推荐的手术切缘并不总是可行的,通常采用较窄的手术切缘(1-3 mm)来缩小手术缺损的大小,尤其是在面部区域,基底细胞癌大多属于高危类型。的确,安全切缘应合理设计,以尽量减少解剖和功能损伤,并尽可能获得最安全的手术切缘,以避免癌症复发
特别是在头颈部区域,肿瘤切除的根治性与健康组织损伤的最小化的需要最近导致了对更窄的安全边界的努力达成一致。事实上,已经有人提出,对于小(≤2cm)界限分明的(结节和浅表型)非形态基底细胞癌,或界限分明的、原发性的、着色的、结节性或浅表基底细胞癌,3mm的手术切缘可安全地用于达到95%的治愈率
在手术中引入皮镜检查,对于更精确地确定肿瘤区域,从而降低安全边缘的范围有很大的帮助。事实上,临床手术切缘的皮肤镜下矫正已被证明为1mm,皮肤镜下肿瘤边界已被证明与组织病理学边界紧密吻合。在本研究中,williamhill asia 的目的是评估皮镜检查是否可以有效地用于减少头颈部界限明确、无侵袭性基底细胞癌手术安全边界的宽度。
材料和方法:回顾性分析切除的较小(≤1 cm)的头颈部基底细胞,比较临床-皮肤镜术前评估(病例)与仅临床评估(对照组)手术切缘的组织学性质和复发情况。
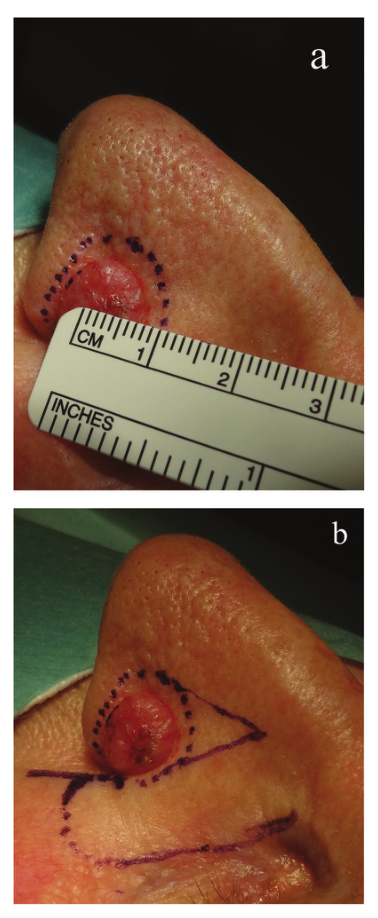
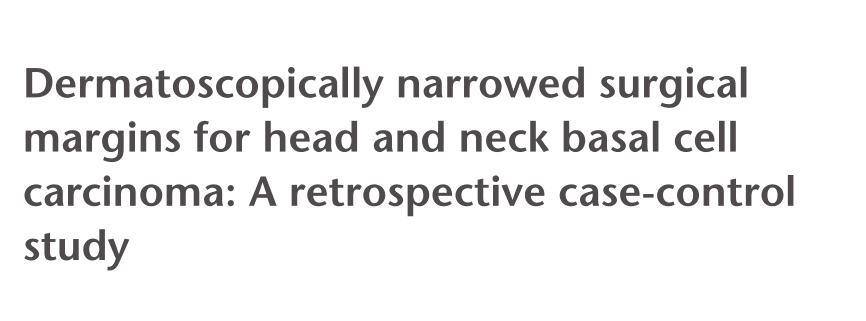
图1 鼻部基底细胞癌(对照,仅临床评估):1.5mm的手术安全切缘由蓝点勾画(a)。1.5mm的临床评估手术切缘(蓝点)和手术计划(蓝色全线)(b)。

图2 额头基底细胞癌(对照,仅临床评估):浅蓝色小点显示3mm的手术安全切缘(a)。浅蓝色全线显示3mm的临床评估手术切缘,被手术计划覆盖(b)。
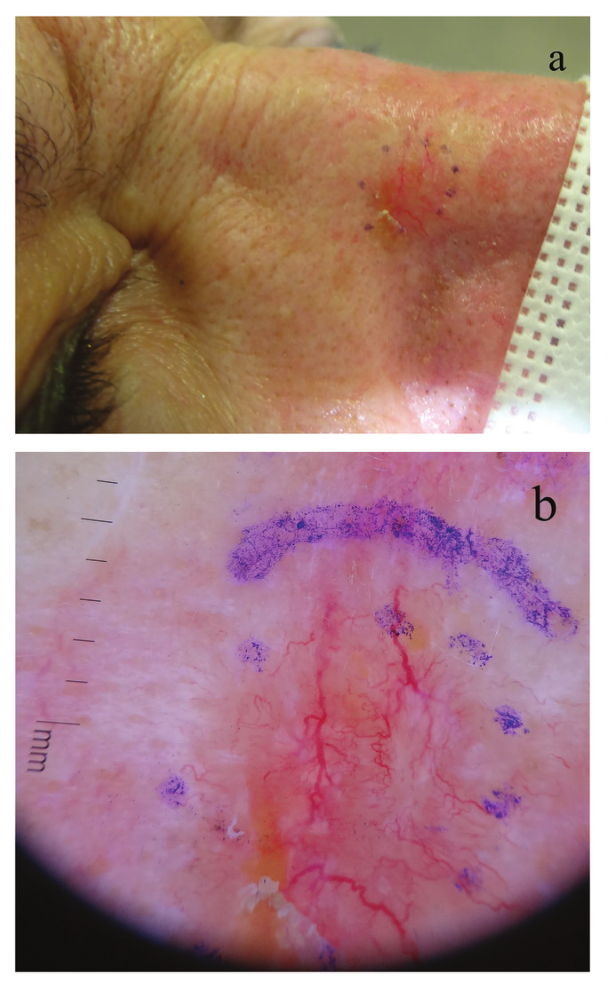
图3 鼻子基底细胞癌(病例):1.5 mm的手术安全切缘首先被临床评估,并用蓝点勾画(a)。1.5 mm的临床评估手术切缘(蓝点)和1.5 mm的皮肤镜评估切缘(蓝色全线)(b)。
结果:281例基底细胞癌中,6%(8/139)的病例和8%(12/142)的对照组深部边缘不正常;4 %(5/139)的病例,20 %(29/142)的对照组侧边切缘不正常(P < 0.001)。3 mm侧切缘不正常的病例占0%(15/66),对照组占15% (10/66)(P > 0.005);手术侧切缘1 ~ 2mm不合适者占7%(5/73),对照组25% (19/76)(P < 0.01)。在3mm、1 - 2mm切除的病例和对照组中,复发率分别为1.5%、0%和7.7%。
结论:头颈部3mm切缘的基底细胞癌切除适合于小的、皮肤镜下明确的、无侵袭性的基底细胞癌,手术治愈率为100%,复发率为1.5%。由于手术治愈率仅为93%,所以1 - 2mm的切除应只保留应用于在非常难以治疗的区域的基底细胞癌。
文献来源:Herzum A, Burlando M, Tavilla PP, Dermatoscopically narrowed surgical margins for head and neck basal cell carcinoma: A retrospective case-control study.J Dtsch Dermatol Ges 2022 Jun;20(6)
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#基底细胞#
52
#细胞癌#
83
认真学习了
76
#头颈部#
55
#颈部#
69