至关重要!结缔组织相关间质性肺病的这项检测不可忽视!
2021-06-21 检验医学网 检验医学网
结缔组织疾病(CTD)是一种以全身血管和结缔组织的慢性非感染性炎症为病理基础的自身免疫性疾病,累及肺脏时可出现间质性肺病。间质性肺疾病(ILD)是一组主要累及肺间质和肺泡腔,导致肺泡、毛细血管功能单位
结缔组织疾病(CTD)是一种以全身血管和结缔组织的慢性非感染性炎症为病理基础的自身免疫性疾病,累及肺脏时可出现间质性肺病。间质性肺疾病(ILD)是一组主要累及肺间质和肺泡腔,导致肺泡、毛细血管功能单位丧失的弥漫性肺疾病的总称。临床主要表现为进行性加重的呼吸困难、通气功能障碍伴弥散功能降低、低氧血症和影像学上的双肺弥漫性病变。
间质性肺病(ILD)是结缔组织疾病(CTD)患者常见的肺部并发症,可见于多种CTD,如系统性硬化症(SSc)、多发性肌炎/皮肌炎(PM/DM)、类风湿关节炎(RA)、干燥综合征(SS)和系统性红斑狼疮(SLE)。患病率因检测方法的不同而差异较大,为3%~70%。不同的CTD-ILD在临床表现、影像学和病理特征上也不尽相同,呈现各自的发展与转归,导致诊断和治疗困难。
表1 CTD相关ILD常见组织病理学和胸部高分辨率CT的影像学特征

CTD-ILD的临床表现和影像学特征与其他类型的ILD相似,因此常被误诊。部分CTD-ILD患者以肺部症状为首发表现时,称为肺显性CTD,这些患者常常被诊断为其他疾病,如特发性肺纤维化(IPF)。然而CTD-ILD和IPF的治疗方案不同,因此准确诊断CTD-ILD对患者预后至关重要。
CTD-ILD患者在初次入院时不能得到准确的诊断的原因,多数是由于自身抗体血清学检测结果阴性以及没有明显的肺外症状。但随着患者病情的进展,肺外症状以及自身抗体转阳的情况逐渐显现,因此需要对ILD患者及时随访观察。
一、自身抗体检测对CTD-ILD 的临床意义
上海肺科医院一项近13年的回顾性研究资料,对大样本量的CTD-ILD患者自身抗体与疾病关系进行了全面分析。具体内容及主要结论如下:
研究针对具有完整临床资料的1044例CTD-ILD患者疾病特点及抗体情况进行统计分析。入组患者均进行了临床表现评估及血清学检测,同时有肺部影像学检测以及肺功能测试和动脉血气分析资料。
血清学抗体检测项目主要包括ANA、抗dsDNA抗体、抗Sm抗体、抗nRNP抗体、抗Ro抗体(SSA)、抗La抗体(SSB)、抗Jo-1抗体、抗Scl -70抗体、抗核小体抗体、抗CENP-B抗体、抗核糖体P蛋白抗体、抗组蛋白抗体、类风湿因子等。包括初检时抗体阴性的患者,每3-6个月定期随访,记录抗体变化情况。
主要结论:
1、肺部为首发临床表现的患者监测抗体的意义更大
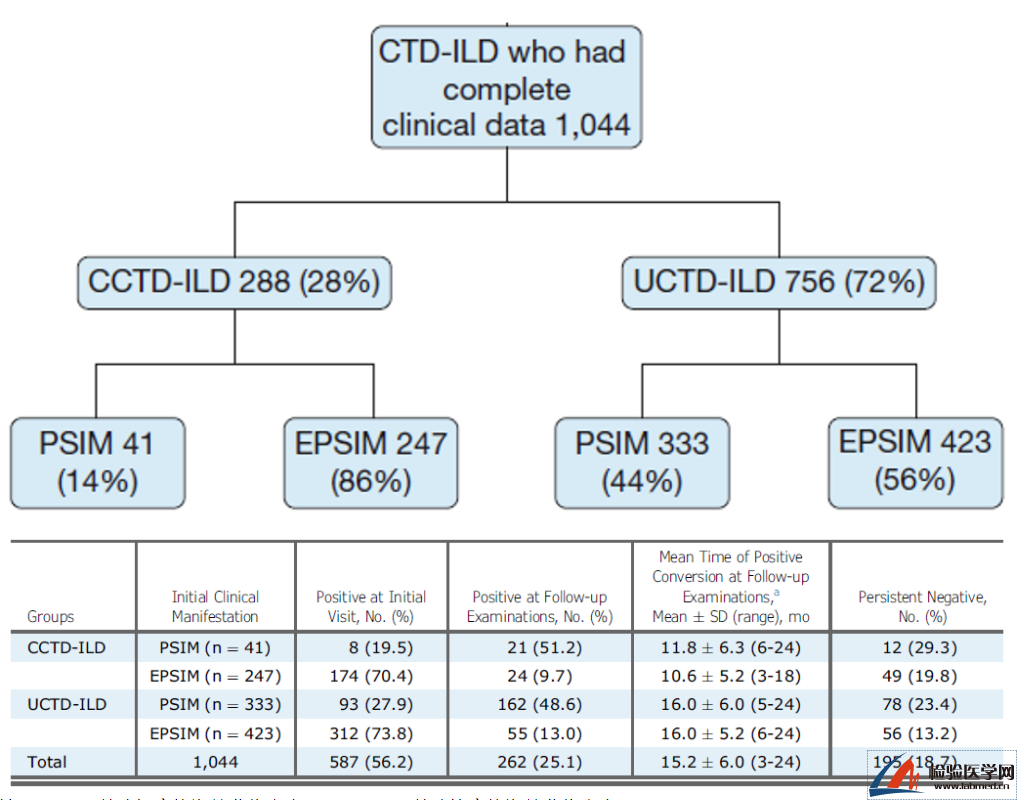
注:PSIM,以肺部症状为首发临床表现;EPSIM,以肺外症状为首发临床表现
在以肺外表现为首发症状(EPSIM)的患者中,首诊时抗体阳性比例较高分别为70.4%和73.8%。以肺部表现为首发症状(PSIM)的患者中,51.2%的CCTD-ILD和48.6%的UCTD-ILD从首次就诊时的阴性转变为随访时的阳性。CCTD-ILD和UCTD-ILD中持续阴性结果的患者比例没有显着差异。
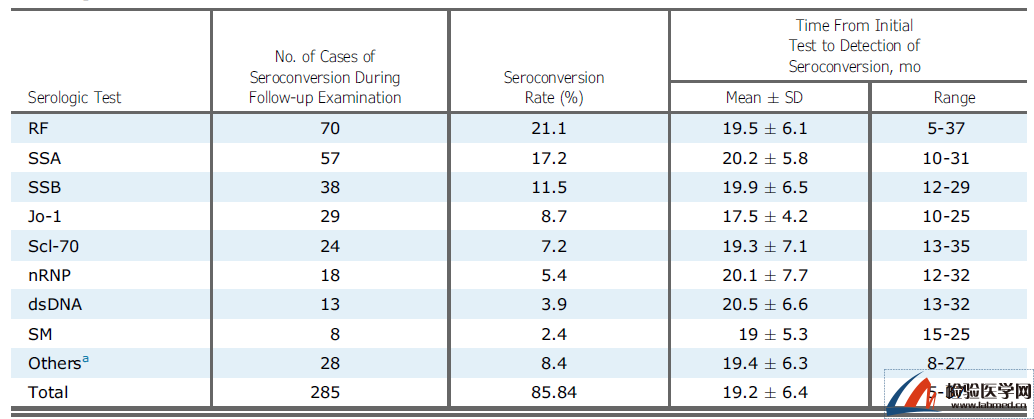
2、从最初诊断到检测血清转化的时间,不同抗体有差异
血清中自身抗体的转化定义为最初诊断时抗体为阴性,在随后的随访检查中测试结果转化为阳性。计算血清中抗体转化率(即随访中发生血清转化的患者百分比)和抗体转化时间(平均值Mean±SD及Range)。在所有的自身抗体检测中,类风湿因子的血清转换百分比最高(21.1%),血清转换为5 ~ 37个月,平均血清转换时间为19.5±6.1个月。
3、ILD患者的CTD诊断,对患者获得良好预后更显重要
从UCTD-ILD组和CCTD-ILD组看,疾病缓解+疾病改善的结果分别为75.1%和77.4%。但也不难发现其中20例死亡病例中有16例(80%)与CTD-ILD急性加重相关。从治疗的角度,抗纤维化治疗联合糖皮质激素、抗风湿疾病治疗对患者是有效的,因此疾病的及时准确诊断,抗体检测作为辅助工具,显得必不可少。

二、小结
由于在CTD-ILD的患者中存在肺部症状先于肺外症状临床表现的情况,一些有肺部症状但特异性抗体为阴性的患者有可能被诊断为特发性间质性肺炎(IPF)。
在上述研究中,32%的患者首诊被诊断为其他ILD;43.8%的患者首次入院时血清学抗体检测结果为阴性(其中包括25.1%随访中血清转阳的患者以及18.7%抗体持续阴性的患者)。
这些证据提示,针对无肺外表现及抗体阴性的ILD患者,在随访过程中不仅要关注肺外体征和症状的变化,同时特异性抗体的检测也不容忽视,抗体性质的转变能够给患者带来及时准确的诊断提示。这也显示了自身抗体检测在肺部疾病诊断中重要的应用价值。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#间质性#
69
#结缔组织#
63
#肺病#
58
创新!
72
非常实用
71
学习
67