Lung Cancer:多西他赛vs多西他赛+厄洛替尼治疗复发晚期非鳞状非小细胞肺癌的疗效:III期临床研究NVALT-18
2021-09-10 yd2015 MedSci原创
该研究表明厄洛替尼的加入并不能改善患者的预后,反而产生不利的影响,并强烈反对在临床实践中进一步探索这种联合。
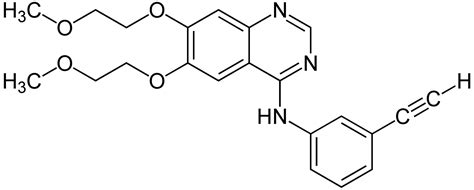
在之前的一项随机II期研究(NVALT-10)中,研究发现联合化疗+厄洛替尼治疗复发晚期非鳞状非小细胞肺癌(NSQ- NSCLC)患者较厄洛替尼单药治疗改善总生存期(OS)。近期,研究开展了一项III期临床研究(NVALT-18:NCT0277500),评估多西他赛vs多西他赛+厄洛替尼治疗复发晚期非鳞状非小细胞肺癌的疗效。相关结果发表在Lung Cancer杂志上。
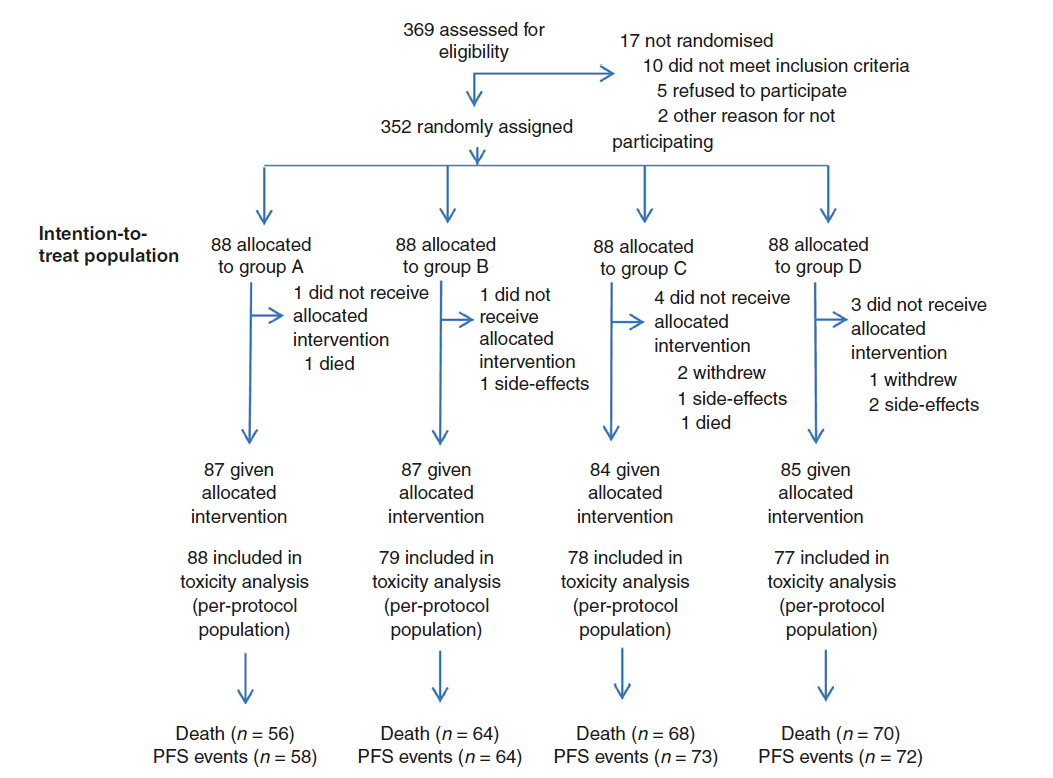
NVALT-18研究是一项前瞻性、多中心、随机、开放III期临床研究,无进展生存期(PFS)是主要终点,次要研究终点是应答持续时间、总生存期(OS)和毒性。
2016年10月至2018年4月,共有45名患者被随机分配,接受了对照组(N = 23)或实验组(N = 22)的治疗,由于累积缓慢,该研究停止。
多西他赛单药组和联合组的PFS分别为4.0个月(95% CI: 1.5 7.1)和1.9个月(95% CI: 1.4 3.5) (调整后HR=2.51, 95% CI: 1.16 5.43, p = 0.01 )。两组的中位OS分别为10.6个月(95% CI: 7.0 8.6) 和4.7个月(95% CI: 3.2 8.6)(调整后HR=3.67,95% CI: 1.46 9.27,p = 0.004)。两组1年生存率分别为43% (95% CI: 26% 74%)和14% (95% CI: 5% 39%)。

两组的PFS和OS
多西他赛单药组和联合组的客观缓解率分别为13% (N = 3)和9% (N = 2)。单药组的3例患者的肿瘤应答持续时间分别为14、19和40周,联合组2例患者的肿瘤应答持续时间分别为8和25周。
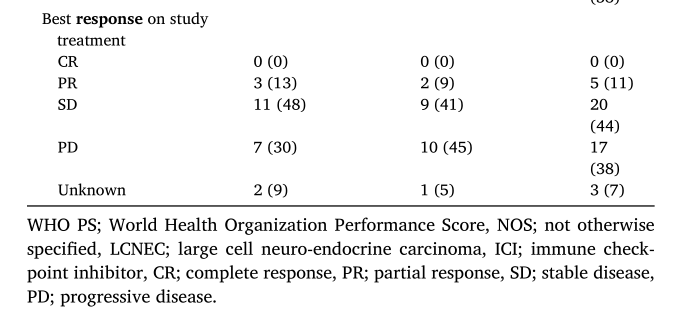
ORR
单药组有6例患者(26%)经历了CTCAE 3级毒性,而联合组有17例患者(77%)(p = 0.0009),主要表现为胃肠道症状和白细胞减少。本研究未见CTCAE 5级AEs报告。

不良反应
综上,该研究表明厄洛替尼的加入并不能改善患者的预后,反而产生不利的影响,并强烈反对在临床实践中进一步探索这种联合。
原始出处:
Steendam CMJ, Peric R, van Walree NC, et al. Randomized phase III study of docetaxel versus docetaxel plus intercalated erlotinib in patients with relapsed non-squamous non-small cell lung carcinoma. Lung Cancer. 2021 Aug 4;160:44-49. doi: 10.1016/j.lungcan.2021.08.002. Epub ahead of print. PMID: 34403911.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#II期临床研究#
103
#III#
64
#I期临床#
67
#非小细胞#
57
#III期临床研究#
63
#ALT#
58
#非鳞状非小细胞肺癌#
63
#厄洛替尼#
67
#II期临床#
56
#III期#
56