J Urol:行机器人肾部分切除术患者中,围手术期服用阿司匹林会造成什么后果?
2021-10-17 AlexYang MedSci原创
评估了RPN期间的围手术期使用阿司匹林(pASA)的结果。
在大手术前是否要停止阿司匹林或其他抗血小板治疗,需要权衡潜在的出血风险和可能增加的血栓事件风险。一项关于阿司匹林在围手术期使用的大型随机临床试验(POISE2)表明大出血风险增加,且死亡或非致命性心肌梗死的风险没有明显降低。然而,POISE2试验的一个亚组分析显示,有经皮冠状动脉介入病史的患者可能会从阿司匹林使用中受益。然而,对于泌尿科医生来说,是否在大手术前停止服用阿司匹林的问题仍然未解。

目前,患者在心血管介入治疗后普遍服用阿司匹林,但阿司匹林会导致出血风险,这也使得患者感到担忧。尽管阿司匹林有保护心脏的作用,但由于出血风险,通常在手术前5-7天就停止使用。已有单机构的研究调查了在行机器人肾脏部分切除术(RPN)患者中使用阿司匹林的围手术期结果。
近期,来自美国的研究人员在《J Urol》杂志上发表文章,他们在一个多中心背景下,评估了RPN期间的围手术期使用阿司匹林(pASA)的结果。

研究人员在5家高容量的RPN机构中,对接受RPN的患者进行了评估。比较了服用pASA(81毫克)和未服用阿司匹患者的围手术期结果。他们还评估了使用pASA和围手术期输血之间的关系。
在1565名接受RPN的患者中,228名(14.5%)患者服用pASA,他们年龄较大(62.8岁 vs. 56.8岁,p<0.001),Charlson评分较高(平均3分 vs. 2分,p<0.001)。pASA与围手术期输血量增加(11% vs. 4%,p<0.001)和重大并发症(10% vs. 3%,p <0.001)的发生有关。在多变量分析中,pASA与输血风险增加有关(OR 1.94,1.10-3.45,95%CI)。
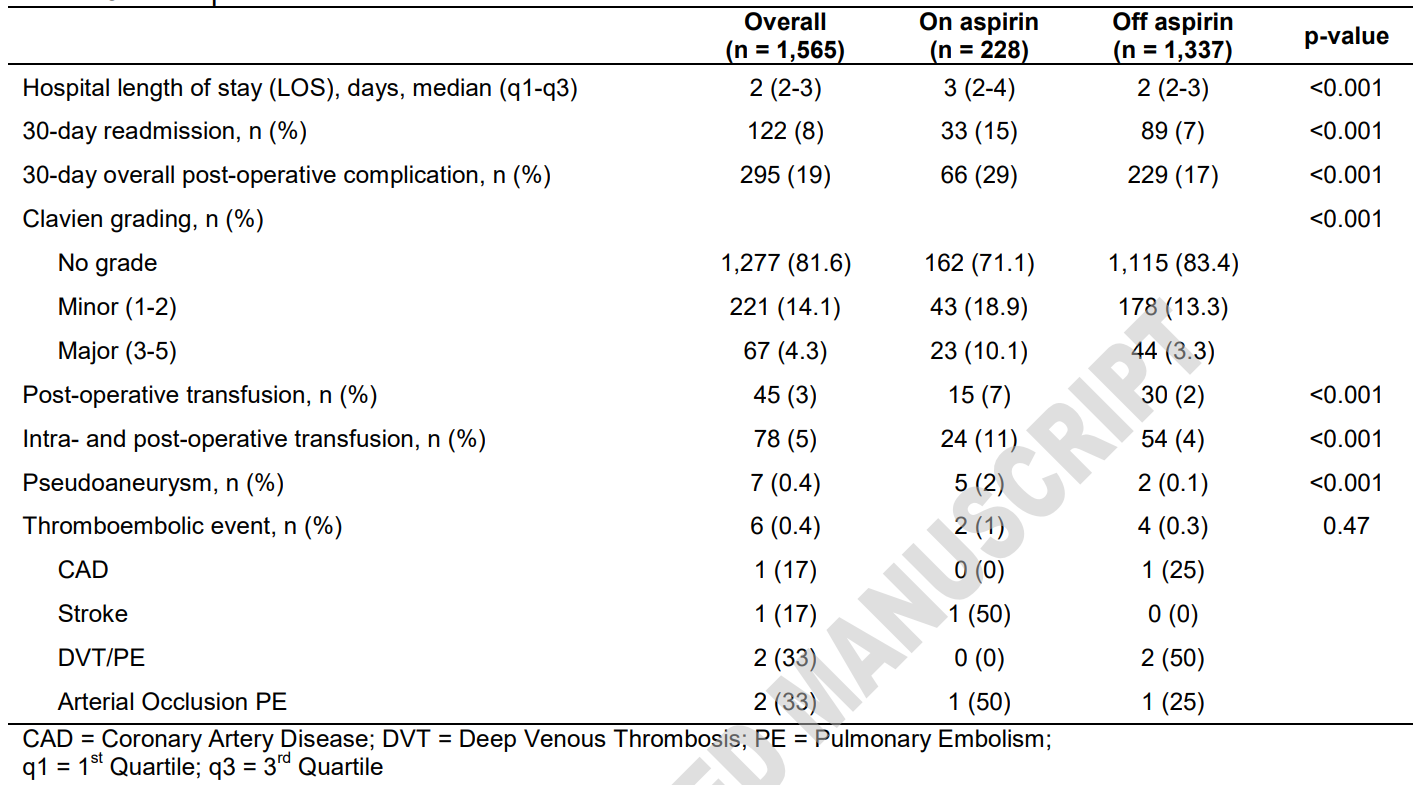
术后结果情况
综上所述,RPN期间的围手术期使用阿司匹林是合理和安全的,然而,有较高的输血和发生重大并发症的风险。另外,在需要pASA的RPN患者中,未来的研究需要明确抗血小板治疗的作用,以更好的实现心血管事件的一级或二级预防。
原始出处:
Joan C Delto, Aaron Fleishman, Peter Chang et al. Perioperative Aspirin Use is Associated with Bleeding Complications During Robotic Partial Nephrectomy. J Urol. Sep 2021
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












分享学习
52
当今社会机器人手术成为趋势,需要更多的关注心血管病患者用药影响
73
感谢分享
55
客观评价
65
学习受益
54
#手术期#
54
#切除术#
50
#机器人#
55
#机器#
49