ASCO威廉亚洲博彩公司 重磅更新!对于HER2阳性晚期乳腺癌,最佳治疗到底是什么?最新最全循证依据也都在这了!
2022-06-02 LILYMED MedSci原创
J Clin Oncol:晚期人表皮生长因子受体2阳性乳腺癌的系统治疗:ASCO威廉亚洲博彩公司 更新
本威廉亚洲博彩公司 更新的目的是为肿瘤学家、其他卫生保健从业人员、患者和护理人员提供有关指导人表皮生长因子受体 2 (HER2) 阳性转移性乳腺癌 (MBC) 患者最佳管理的建议。
ASCO 于 2014 年首次发布了两份关于 HER2 阳性 MBC 患者最佳管理的循证临床实践威廉亚洲博彩公司
,并于 2018 年更新了威廉亚洲博彩公司
。本威廉亚洲博彩公司
更新的目的是为肿瘤学家和其他临床医生提供有关 HER2 阳性 MBC 患者治疗的当前建议。当前更新评估了 2018 年的建议是否仍然有效。

指导问题
对于晚期人表皮生长因子受体2(HER2)阳性乳腺癌,特别是HER2靶向治疗,单独或与化疗和/或内分泌治疗联合使用的最佳药物治疗是什么?
目标人群
晚期 HER2 阳性乳腺癌患者。
目标受众
肿瘤内科医生、放射肿瘤学家、外科医生、肿瘤科护士、患者和护理人员。
主要更新建议
一线
建议1.1.
临床医生应推荐曲妥珠单抗、帕妥珠单抗和紫杉烷联合用于一线治疗,除非患者有紫杉烷禁忌证(类型:循证,利大于弊;证据质量:高;推荐强度:强)。无更改。
二线
建议2.1.
如果患者的HER2阳性晚期乳腺癌在一线HER2靶向治疗期间或之后进展(并且患者尚未接受德喜曲妥珠单抗[T-Dxd]),临床医生应推荐T-Dxd作为二线治疗(类型:循证,利大于弊;证据质量:中等;推荐强度:强)。新增/已更改。
三线或更后
建议3.1.
如果患者的 HER2 阳性晚期乳腺癌在二线或更高 HER2 靶向治疗期间或之后进展,并且患者已接受帕妥珠单抗和 T-Dxd 治疗(如果患者未接受帕妥珠单抗,临床医生可能会提供帕妥珠单抗),临床医生应推荐三线或更高程度的基于 HER2 靶向治疗的治疗。
总体而言,目前缺乏头对头试验,因此没有足够的证据推荐一种方案优于另一种方案。在决策过程中,患者和临床医生应讨论治疗方案、途径和毒性的差异。选项包括:
- 如果患者在二线治疗中未接受恩美曲妥珠单抗(T-DM1),应提供T-DM1方案(类型:循证,利大于弊;证据质量:高;推荐强度:强)。新建。
- 可能提供图卡替尼联合曲妥珠单抗和卡培他滨(类型:循证,利大于弊;证据质量:中等;推荐强度:强)。新建。
- 可能提供T-Dxd(类型:基于证据,利大于弊;证据质量:中等;推荐强度:强)。新建。
- 可能提供奈拉替尼联合卡培他滨(类型:循证,利大于害;证据质量:中等;推荐强度:弱)。新建。
- 可能提供拉帕替尼和曲妥珠单抗(类型:循证,利大于弊;证据质量:中等;推荐强度:弱)。
- 可能提供拉帕替尼和卡培他滨(类型:循证,利大于弊;证据质量:中等;推荐强度:弱)。
- 可能提供化疗和曲妥珠单抗的其他组合(类型:循证,益处大于危害;证据质量:中等;推荐强度:弱)。
- 可能提供马格妥昔单抗加化疗(类型:循证,益处大于危害;证据质量:中等;推荐强度:弱)。新建。
- 可能提供激素治疗(在雌激素受体阳性 [ER+] 和/或孕激素受体阳性 [PgR+] 疾病患者中;类型:循证,利大于弊;证据质量:中等;推荐强度:弱)。
- 可能提供阿贝西利与曲妥珠单抗和氟维司群的组合(类型:基于证据,益处大于危害;证据质量:中等;推荐强度:弱)。新建。
- 如果患者没有接受帕妥珠单抗,临床医生可能会提供帕妥珠单抗(类型:非正式共识,利大于弊;证据质量:不足;推荐强度:弱)。无更改。
激素受体阳性 MBC 患者的建议保持不变:基于 HER2 靶向治疗的组合推荐用于同时存在 HER2+ 和激素受体阳性 MBC 的患者。
如果患者的癌症是 ER+ 和/或 PgR+ 和 HER2 阳性,则:
- HER2靶向治疗加化疗或内分泌治疗加曲妥珠单抗或拉帕替尼(在特定病例中)或单独使用内分泌治疗(在特定病例中)。
- 如果患者开始进行HER2阳性靶向治疗和化疗组合,当化疗结束时和/或癌症进展时,临床医生可以在HER2靶向治疗的基础上增加内分泌治疗。
- 限定性声明:尽管临床医生可能会讨论使用联合或不联合 HER2 靶向的内分泌治疗,并且大多数患者仍应接受化疗加 HER2 靶向治疗。
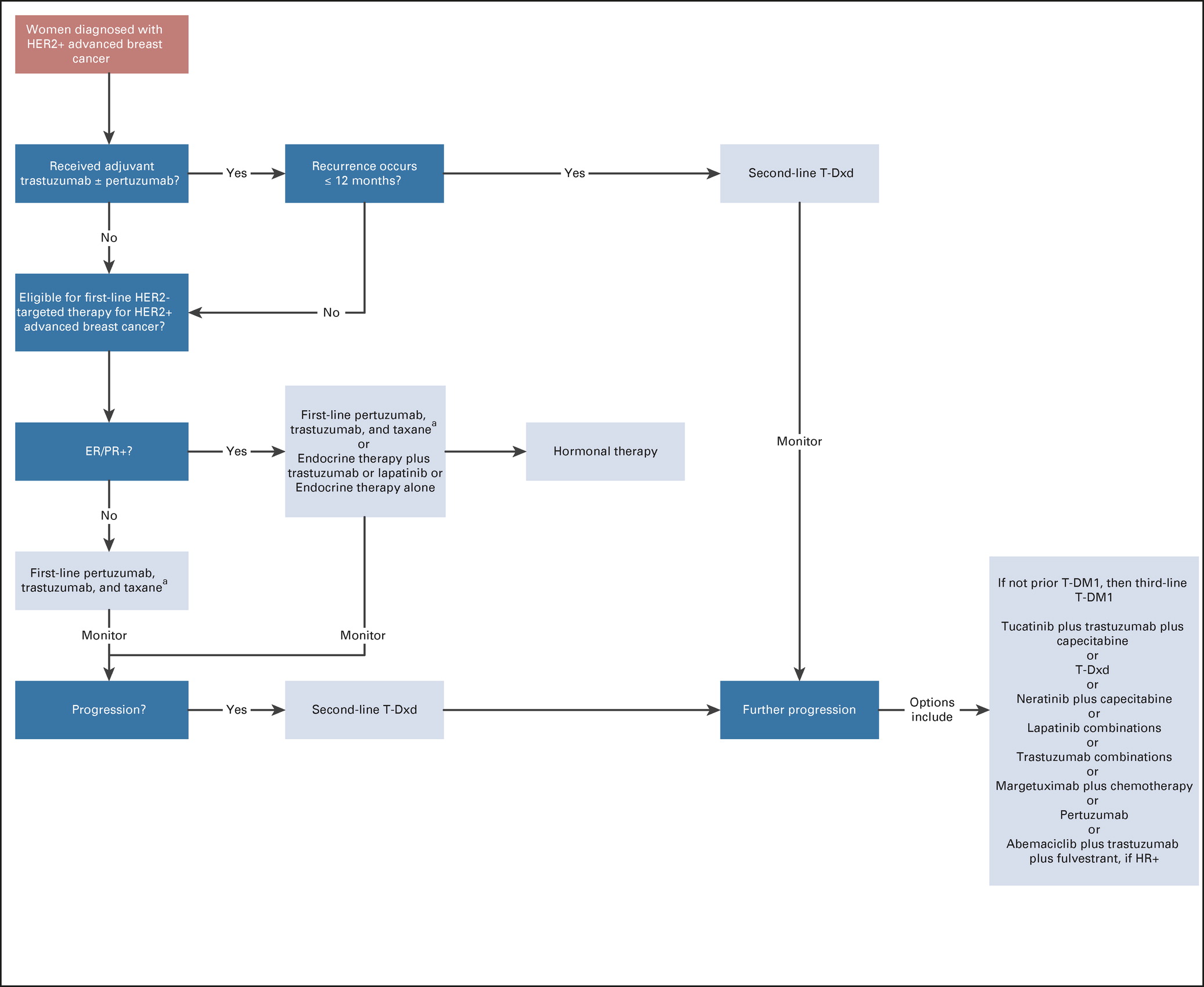
自该威廉亚洲博彩公司 的上一个版本以来,MBC的治疗已经取得了相当大的进展,最终导致美国食品和药物管理局(FDA)批准了三种新的抗HER2方案。推荐的一线治疗方案保持不变,二线治疗方案有一个新选项,三线治疗方案有几种新的和既往的选择。总体而言,没有足够的证据推荐一种方案优于另一种方案,并且抗 HER2 药物在三线和更高线药物中的最佳序列尚不清楚。在选择治疗方案时,医生应考虑疗效结果和治疗方案概况,包括给药途径(口服 v 静脉注射 [IV])、时间表、毒性以及可及性。当患者出现脑转移瘤时,专家小组倾向于在三线治疗中使用图卡替尼、曲妥珠单抗和卡培他滨。在未来的临床研究中,应探讨将图卡替尼、卡培他滨和曲妥珠单抗作为脑转移患者的二线治疗方案。配套威廉亚洲博彩公司 涉及 HER2 阳性晚期乳腺癌和脑转移瘤的治疗。在三线或更后线中,对于既往未接受过激素治疗的激素受体阳性患者,内分泌治疗可能是更好的选择。
原文来源:
https://ascopubs.org/doi/full/10.1200/JCO.22.00519
Giordano SH, Franzoi MAB, Temin S, Anders CK, Chandarlapaty S, Crews JR, Kirshner JJ, Krop IE, Lin NU, Morikawa A, Patt DA, Perlmutter J, Ramakrishna N, Davidson NE. Systemic Therapy for Advanced Human Epidermal Growth Factor Receptor 2-Positive Breast Cancer: ASCO Guideline Update. J Clin Oncol. 2022 May 31:JCO2200519. doi: 10.1200/JCO.22.00519. Epub ahead of print. PMID: 35640077.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#HER2阳性晚期乳腺癌#
100
#ASC#
64
#最新#
81
#HER2阳性#
92
#循证#
62
#重磅#
67