Cell:患者Tau蛋白修饰图谱可以识别阿尔兹海默症分期
2020-11-14 haibei MedSci原创
最近,为了阐明Tau亚型和翻译后修饰(PTM)的计量学在阿尔茨海默病(AD)中的作用,研究人员从49名AD和42名对照组受试者的死后人类组织中分离出了Tau的多种亚型
已有的研究显示,阿尔兹海默症患者脑内具有大量病理性Tau蛋白的聚积。Tau蛋白聚积被认为参与了阿尔兹海默症的发生和进展。针对病理性Tau进行清除的方法有希望成为阿尔兹海默症患者的新型治疗手段。

最近,为了阐明Tau亚型和翻译后修饰(PTM)的计量学在阿尔茨海默病(AD)中的作用,研究人员从49名AD和42名对照组受试者的死后人类组织中分离出了Tau的多种亚型,并研究了这些亚型上面的95个翻译后修饰(PTM)的高分辨率定量蛋白质组学图。
虽然Tau PTM图揭示了不同受试者的异质性,但有一个PTM子集显示出AD的高占有率和频率,表明其在疾病中的重要性。
无监督分析表明,PTMs以有序方式发生,导致Tau聚集。通过对大小分化的Tau的分析,研究人员进一步确定了与tau传播相关的PTMs的过程性添加和最小集合。
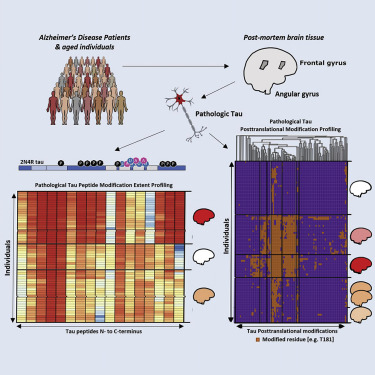
综上所述,该研究确定了Tau蛋白在疾病不同阶段对疾病干预至关重要的特征,包括0N和4R异构体的富集,C端代表性不足,富脯氨酸区(PRR)负电荷增加,微管结合域(MBD)正电荷减少。
原始出处:
Hendrik Wesseling et al. Tau PTM Profiles Identify Patient Heterogeneity and Stages of Alzheimer’s Disease. Cell (2020). DOI:https://doi.org/10.1016/j.cell.2020.10.029
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#Cell#
66
#CEL#
44
#阿尔兹海默#
44
#Tau#
48
#修饰#
70
很不错
0