Stroke:让LDL-C“背锅”的残余胆固醇变异性和缺血性卒中发生密切相关!
2022-05-19 网络 网络
残余胆固醇,而非LDL-C或许才是引起ASCVD的罪魁祸首。
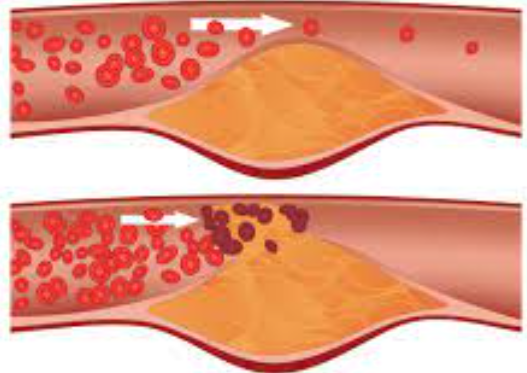
作为动脉硬化这一病变的核心驱动力——LDL-C是所有威廉亚洲博彩公司 中一级与二级预防的主要治疗目标。
然而,最近发表在《美国心脏病学会杂志》(JACC)上的两项大型研究则激起了大家上述认知的争议:残余胆固醇,而非LDL-C或许才是引起ASCVD的罪魁祸首。残余胆固醇(Remnant-C)被定义为除了LDL-C和HDL-C外,人体内包括VLDL-C与中密度脂蛋白胆固醇(IDL-C)等两种胆固醇的含量。

然而,残余胆固醇浓度的逐次变化是否影响缺血性脑卒中尚不清楚。为此,有学者试图研究残余胆固醇的变异性在普通人群中缺血性卒中的后续发展中的作用,结果发表在stroke杂志上。
该研究是一项事后分析,包括开滦研究队列中符合条件的参与者,他们在2006年至2010年期间接受了3次健康检查,没有心房颤动、心肌梗死、中风、癌症或已知的脂质药物使用。参与者被随访至2017年底。
最终的研究队列包括38 556名参与者。经过7.0年的中位随访,1058人被新诊断为缺血性卒中。在调整了年龄(时间尺度)、性别、吸烟状况、饮酒、体力活动、高血压、糖尿病、心血管疾病家族史、身体质量指数、估计肾小球滤过率、低密度脂蛋白胆固醇、高密度脂蛋白胆固醇。
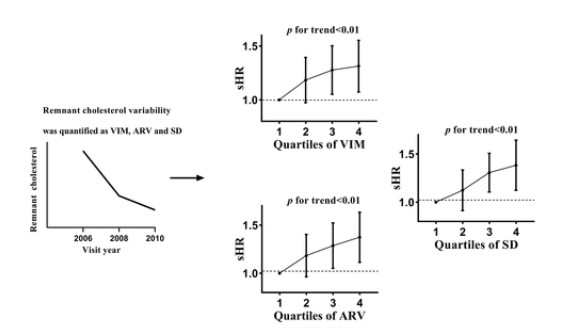
与最低的四分位数(四分位数1)相比,独立于残余胆固醇平均值的最高四分位数(四分位数4)与缺血性卒中风险的增加有关,(HR=1. 27[95%CI,1.06-1.53])。独立于残余胆固醇平均值的变异性每增加1个SD,风险增加9%(HR=1.09[95% CI,1.03-1.16])。
综上,在普通人群中,较大的残余胆固醇变异性与较高的缺血性卒中风险有关。
参考文献:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
















#缺血性#
78
#缺血性卒#
63
学习了,比较新
75
学习了
73
#残余胆固醇#
65
#变异#
62
#LDL#
67