EUR J Cancer:一项比较SB3(曲妥珠单抗生物类似物)和曲妥珠单抗的III期临床研究
2018-02-26 MedSci MedSci原创
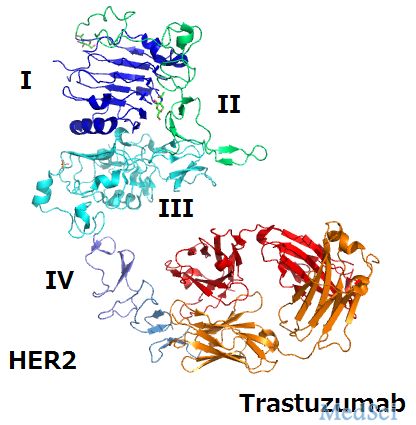
在早期或局部晚期人表皮生长因子受体2阳性乳腺癌患者的治疗中,研究人员对比了SB3(曲妥珠单抗生物类似物)和曲妥珠单抗的在最终安全性,免疫原性和生存结果等方面的差异。
在早期或局部晚期人表皮生长因子受体2阳性乳腺癌患者的治疗中,研究人员对比了SB3(曲妥珠单抗生物类似物)和曲妥珠单抗的在最终安全性,免疫原性和生存结果等方面的差异。
患者被随机平均分配为两组,分别接受SB3或曲妥珠单抗治疗 8个周期,同时进行化疗(4个周期的多西他赛,然后4个周期的5-氟尿嘧啶/ epirubicin /环磷酰胺)。在随机分配的875例患者中,764例(SB3,n = 380;曲妥珠单抗,n = 384)完成了研究。中位随访时间分别为437天(SB3组)和438天(曲妥珠单抗组)。在整个研究期间,各组间治疗出现不良事件的发生率相当(SB3,97.5%;曲妥珠单抗,96.1%)。在研究结束时,两个治疗组的抗药物抗体总发生率较低。12个月时的无事件存活率(EFS)率为93.7%(SB3)和93.4%(曲妥珠单抗)。风险比(SB3 / 曲妥珠单抗)为0.94(95%的置信区间为0.59-1.51)。
原始出处:
本文系williamhill asia
医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#曲妥珠#
43
#III期临床研究#
49
#III#
29
#II期临床研究#
51
#曲妥珠单抗生物类似物#
48
#I期临床#
42
#II期临床#
38
#III期#
53