Blood:Brentuximab vedotin联合苯达莫司汀作为一线补救疗法用于复发性/难治性HL的疗效和安全性
2018-05-02 MedSci MedSci原创
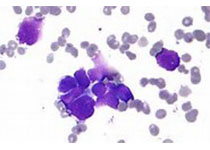
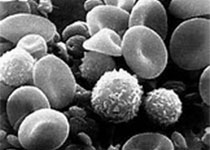
自体干细胞移植(ASCT)是一线化疗后复发/难治性霍奇金淋巴瘤(HL)的标准治疗。预ASCT补救化疗获得完全缓解(CR)预示ASCT后可取得良好预后。Ann S. LaCasce等人开展1/2期研究评估Brentuximab vedotin联合苯达莫司汀作为一线补救疗法用于复发性/难治性HL的疗效和安全性。共招募55位患者(28位原发难治性、27位复发性)。用药方案:BV 1.8mgkg(第一天)
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#mAb#
50
#复发性#
47
#疗效和安全性#
52
学习了谢谢分享!!
93
#Brentuximab#
55
#vedotin#
55
#难治性#
50
#苯达莫司汀#
0
谢谢williamhill asia 提供这么好的信息,学到很多
69
好好学习天天向上
85