JAMA Neurology:脑卒中后,使用氟西汀是否能有效缓解抑郁症状?
2021-09-05 Freeman MedSci原创
与安慰剂相比,每天使用20毫克氟西汀的常规治疗并没有减少中风后出现临床显著抑郁症状的人的比例,也没有影响开抗抑郁药或接受非药物治疗的人的比例。
在中风后的第一年,每3人中就有1人受抑郁症影响。试验的证据表明,使用抗抑郁药可以降低卒中后抑郁症的发病率,尽管研究的数量、规模和质量都很有限,难以推广。
盐酸氟西汀是一种广泛使用的选择性5-羟色胺再摄取抑制剂,在治疗成人抑郁症方面比安慰剂更有效,由于FLAME(Fluoxetine for Motor Recovery After Acute Ischaemic Stroke)试验的结果,它在管理抑郁症风险人群(如中风幸存者)方面的作用引起了人们的兴趣。
FLAME试验随机分配了118名最近中风的成年人,让他们每天接受20毫克的氟西汀或安慰剂治疗,为期3个月。与安慰剂相比,氟西汀治疗增强了运动恢复,并减少了抑郁症患者的比例(7% vs 29%)。
一项系统回顾总结了6项小型研究的结果,调查了氟西汀对中风患者情绪的影响,但只有2项研究是安慰剂对照的。Dam等人随机分配中风患者每天接受盐酸氟西汀20毫克(n = 16)或安慰剂(n = 16)。
3个月后,治疗组在汉密尔顿抑郁症评定量表的得分上没有差异。Robinson等人随机分配27名中风成人接受盐酸氟西汀(每天≤40毫克),28名接受安慰剂,为期12周。他们发现,与安慰剂相比,氟西汀并没有改善没有抑郁症的参与者的病情,而且可能使基线上有抑郁症的人的病情恶化。
最近,3项大型随机、双盲、安慰剂对照的临床试验研究了氟西汀对中风患者的影响,其中抑郁症被记录为次要的结果。FOCUS(Fluoxetine or Control Under Supervision)试验随机抽取了3127名成人,EFFECTS(Efficacy of Fluoxetine-a Randomised Controlled Trial in Stroke)随机抽取了1500名参与者,AFFINITY(Assessment of Fluoxetine in Stroke Recovery)试验随机抽取了1280名参与者,每天接受20mg盐酸氟西汀或相应的安慰剂治疗6个月。
氟西汀没有改善功能结果,但FOCUS和EFFECTS发现,氟西汀降低了抑郁症的发生率。
这些研究中使用的抑郁症的实用性定义,具有不确定的有效性(非结构化的临床医生对抑郁症的诊断non-structured clinician diagnosis of depression)。
西澳大利亚的Osvaldo P. Almeida等人,假设:氟西汀的治疗能够降低那些在基线上有明显抑郁症症状的人的临床显著症状的发生率,以及那些在试验开始时,没有临床显著抑郁症症状的人,降低其临床抑郁症的累积发生率。
主要临床问题:研究每天使用20mg的盐酸氟西汀治疗是否能减少中风后出现临床显著抑郁症状的人的比例。
在这个平行组、随机(1:1分配)、双盲、安慰剂对照临床试验的二级分析中,2013年1月11日至2019年6月30日在澳大利亚、新西兰和越南招募了1221名参与者,并随访了6个月。18岁或以上的成年人在经历了与改良的Rankin量表评分为1或更高的中风后2至15天被招募。
干预措施。盐酸氟西汀,20毫克,或匹配的安慰剂,持续26周。
通过患者健康调查问卷(PHQ-9),得分9分或更低是试验中预先指定的次要结果。评估在基线和4、12和26周时完成。其他相关结果包括参与者报告的临床医生对抑郁症的诊断,非试验性抗抑郁药的处方,或对抑郁症的非药物治疗。分析是在有意治疗的基础上进行的。
他们发现:共有607名参与者(378名男性[62.3%];平均[SD]年龄,64.3[12.2]岁)被随机分配到安慰剂治疗,614名参与者(397名男性[64.7%];平均[SD]年龄,63.4[12.4]岁)被随机分配到每天20mg的盐酸氟西汀治疗。
在基线时,安慰剂组的112名患者(18.5%)和氟西汀组的116名患者(18.9%)的PHQ-9评分为9分或以上。
在随访期间,接受安慰剂治疗的596名参与者中有126人(21.1%)和接受氟西汀治疗的598名参与者中有121人(20.2%)的PHQ-9评分为9分或以上(P=0.70)。
在试验期间,基线时PHQ-9评分低于9分的参与者中,盐酸氟西汀和安慰剂的比例相似,PHQ-9评分达到9分或更高。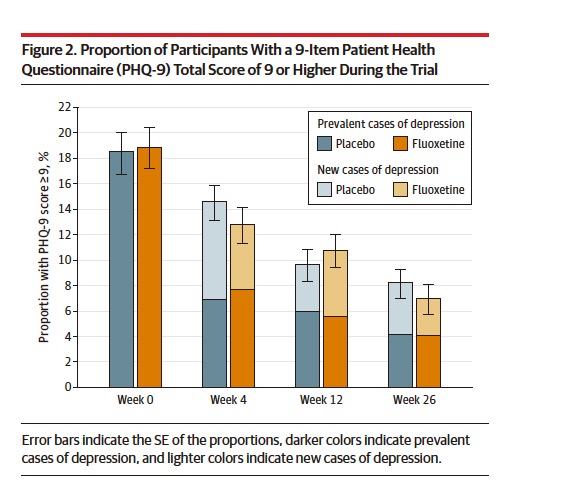
安慰剂组比氟西汀组相比,临床医生诊断为抑郁症的人数略高(602人中有42人[7.0%],601人中有26人[4.3%];P=.05)。
到第26周,安慰剂组的14名参与者(2.3%)和氟西汀组的12名参与者(1.9%)已经死亡(P = .67)。
这个RCT研究的重要意义在于发现了:与安慰剂相比,每天使用20毫克氟西汀的常规治疗并没有减少中风后出现临床显著抑郁症状的人的比例,也没有影响开抗抑郁药或接受非药物治疗的人的比例。
原文出处:
Almeida OP, Hankey GJ, Ford A, et al. Depression Outcomes Among Patients Treated With Fluoxetine for Stroke Recovery: The AFFINITY Randomized Clinical Trial. JAMA Neurol. Published online August 2, 2021. doi:10.1001/jamaneurol.2021.2418
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
















#Neurol#
67
#卒中后#
48
学习
81
#抑郁症状#
68
学习了
67
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
80
顶刊就是顶刊,谢谢williamhill asia 带来这么高水平的研究报道,williamhill asia 科里同事经常看williamhill asia ,分享williamhill asia 上的信息
82