JAHA:社区暴力犯罪与心血管疾病死亡率之间的关系
2022-07-17 MedSci原创 MedSci原创
从2000年到2014年,芝加哥社区暴力犯罪率的大幅下降与心血管疾病和冠状动脉疾病死亡率的大幅下降有关。
最近,美国许多大城市的暴力犯罪都有所增加。先前的研究表明,社区犯罪水平与心血管疾病之间存在关联,但许多研究都受到了横断面设计的限制。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员分析了暴力犯罪率的纵向变化是否与社区水平心血管死亡率的变化相关。
美国芝加哥由77个社区组成,研究人员对2000-2014年社区心血管疾病、卒中和冠状动脉疾病的年龄调整死亡率,每5年汇总一次,数据来自伊利诺伊州公共卫生部门生命记录司。按社区划分的平均总犯罪率和暴力犯罪率来自芝加哥市警察数据门户网站,并通过使用双向固定效应估计。研究人员评估了2000年至2014年社区区域层面的人群、经济变量变化和长期时间趋势后,暴力犯罪纵向变化与心血管死亡率之间的关联。
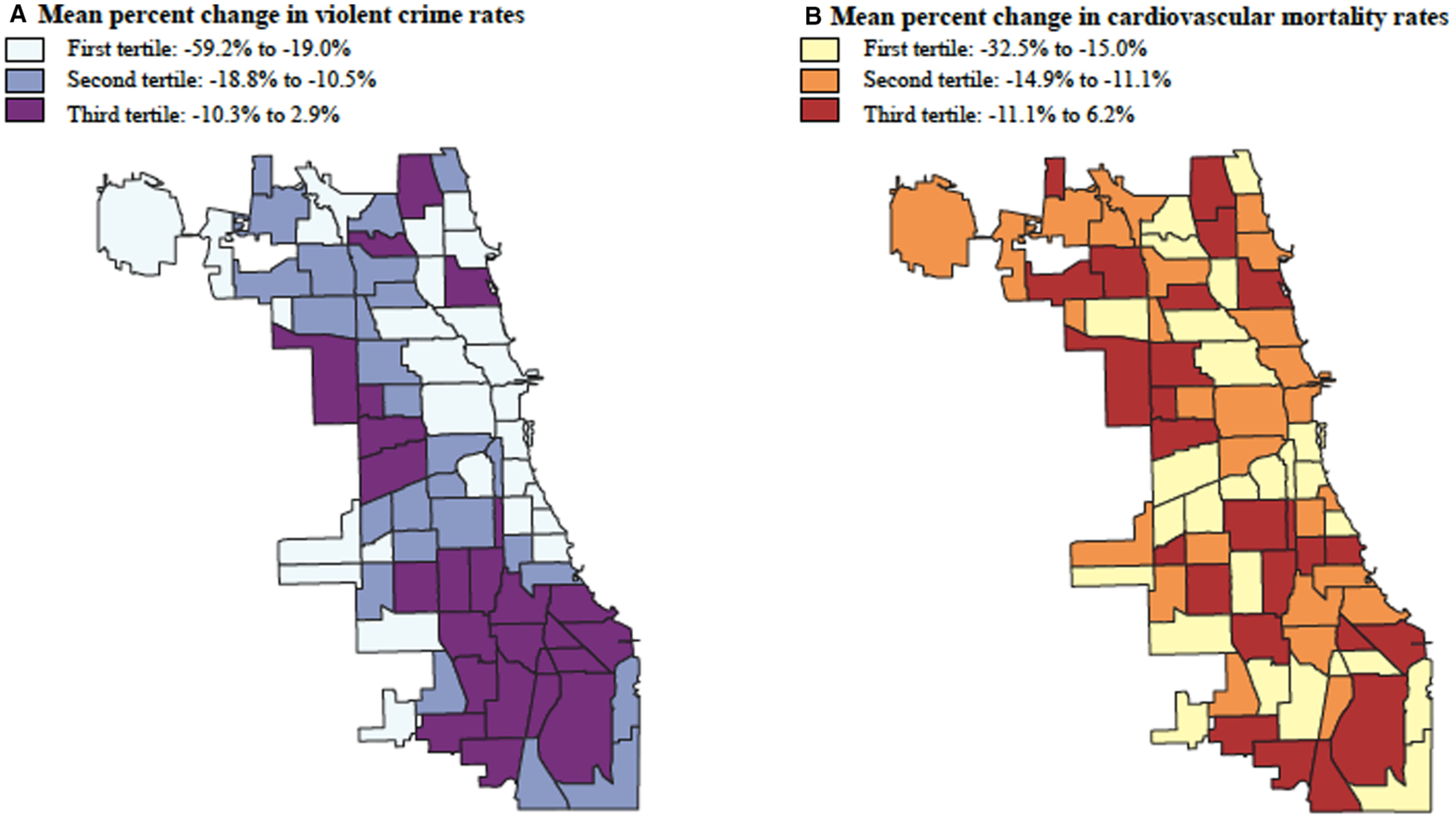
2000年至2014年间,芝加哥的暴力犯罪率中位数从2000年至2004年间的每10万人中3620人(四分位差范围为2256-7777)下降到2010年至2014年间的每10万人中2390人(四分位差范围为1507-5745)(趋势P=0.005)。在固定效应模型中,社区暴力犯罪率下降1%与心血管疾病死亡率下降0.21%(95%CI为0.09-0.33)和冠状动脉疾病死亡率下降0.19%(95%CI为0.04-0.33)相关(P=0.01)。暴力犯罪的变化与卒中死亡率之间没有统计学上的显著关联(-0.17%[95%CI为-0.42-0.08;P=0.18)。
由此可见,从2000年到2014年,芝加哥社区暴力犯罪率的大幅下降与心血管疾病和冠状动脉疾病死亡率的大幅下降有关。这些结果为维持社会治安环境对健康的影响提供了越来越多的证据,并表明暴力犯罪是心血管健康的潜在社会决定因素。对社区进行有针对性的投资以减少暴力犯罪,可改善社区心血管健康。
原始出处:
Lauren A. Eberly.et al.Association Between Community‐Level Violent Crime and Cardiovascular Mortality in Chicago: A Longitudinal Analysis.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.122.025168
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#暴力犯罪#
59
#AHA#
58
#社区#
61
#血管疾病#
76