NEJM:空气支气管征-案例报道
2015-12-31 MedSci MedSci原创
http://www.nejm.org/doi/full/10.1056/NEJMicm1503806
女性,26岁,既往有狼疮性肾炎演变成终末期肾脏病史,今因出现发烧、咳嗽和气短3天余而来院就诊。
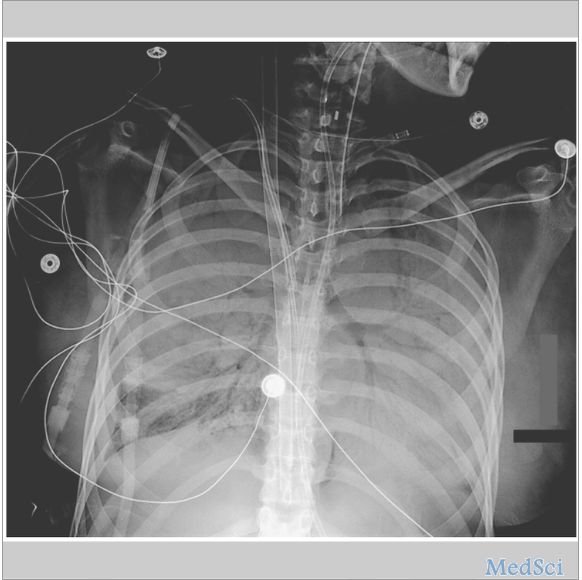
床边X线胸片检查结果显示,双侧胸廓呈现大范围的实质病变,与相邻的含气支气管形成鲜明的对比。
作支气管支纤镜检查肺泡灌洗液培养,培养结果显示卡他莫拉菌和流感嗜血杆菌感染。
随后,该患者遵医嘱应用抗生素进行治疗,同时,还接受血液透析及其他支持性的治疗。
9天后,该患者成功暂停体外膜肺通气(ECMO),并于4天前脱离呼吸机自主呼吸。
出院后,在6个月的随访中,该患者康复良好。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#支气管#
41
双肺几乎完全实变,还被救活了,主要归功于体外膜氧合
132
不错,赞一个
57
这篇文章有一定深度
164
是一篇不错的文章
115
值得进一步关注
58
学会了
80
ECOMO
126
看看
120