Stroke:高密度脂蛋白胆固醇与总的、缺血性和出血性卒中发生率的U型关系
2022-01-30 MedSci原创 MedSci原创
较低和较高的平均累积HDL-C均与缺血性卒中和出血性卒中风险增加相关。
大多数的研究提示甘油三脂水平升高与缺血性卒中发生风险增加密切相关,但是,高密度脂蛋白胆固醇(HDL-C)水平与卒中之间的关系存在相互矛盾的地方。近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,在这一项前瞻性队列研究中,研究人员旨在调查连续测量的HDL-C水平与卒中风险之间的关联。

研究人员纳入了96258名个体(79.6%为男性,平均年龄为51.5岁),在开滦研究中,受试者基线时没有卒中、心肌梗死或癌症病史,并在2006年、2008年、2010年、2012年、2014年和2016年重复测量了HDL-C水平。
研究人员使用所有可用的HDL-C测量值在卒中发生或随访(2017年12月31日)结束之前计算了平均HDL-C浓度。研究人员通过查阅病历确认了卒中病例,并进一步细分为缺血性或出血性卒中。研究人员采用Cox比例风险回归和限制三次样条评估了这些关联。
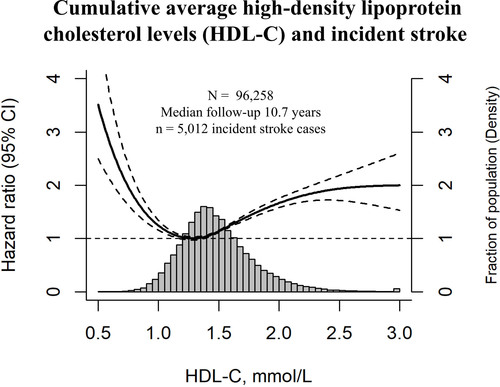
在10.7年的中位随访期间,该研究共发生了5012例卒中事件。受限三次样条分析表明,累积平均HDL-C浓度与卒中风险之间存在U型关联(非线性P<0.001),风险最低值为1.29mmol/L。在调整心血管危险因素后,累积平均HDL-C≤1.06mmol/L或≥2.05mmol/L个体的总卒中风险比为1.31(95%CI为1.15-1.49)和1.85(1.63-2.09),相比于HDL-C为1.26至1.39mmol/L的个体。缺血性卒中的相应风险比分别为1.29(1.11-1.48)和1.84(1.60-2.11),出血性卒中的相应风险比分别为1.54(1.12-2.12)和2.29(1.73-3.04)。
由此可见,较低和较高的平均累积HDL-C均与缺血性卒中和出血性卒中风险增加相关。
原始出处:
Haibin Li.et al.U-Shaped Relationship of High-Density Lipoprotein Cholesterol and Incidence of Total, Ischemic and Hemorrhagic Stroke: A Prospective Cohort Study.stroke.2022.https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.034393
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#发生率#
65
牛的
89
#缺血性#
72
#出血性卒中#
82
#脂蛋白#
0
#高密度脂蛋白胆固醇#
95
杂志Stroke上发表了一篇研究文章,
130
学习了,谢谢分享
116
学习了
113
学习
113