Prostate:转移性前列腺癌相关的P62能够抑制自噬流和促进上皮间质转化
2018-02-18 AlexYang MedSci原创
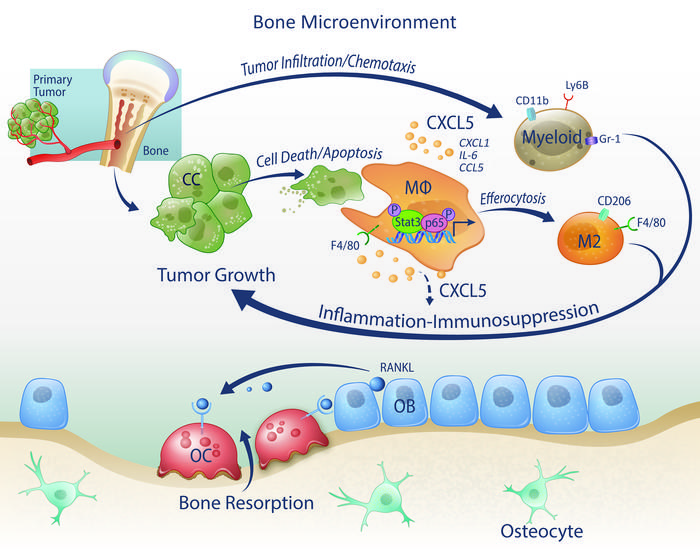
P62可以通过多种路径参与细胞自噬。P62在自噬体中与自噬体相关的LC3-II和泛素化蛋白聚合体互作从而吞噬聚合物,还可与HDAC6互作来抑制它的脱乙酰酶活性来维持乙酰化α-微管蛋白水平和微管的稳定性来增强自噬体转运,并且还可以调节自噬起始和细胞生存。最近,有研究人员在来源于前列腺癌病人的前列腺组织中进行了P62免疫组化染色,发现P62在患有前列腺腺癌(PCA)的病人中的水平要比那些患有良性前列腺
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#上皮间质转化#
54
#ROS#
48
#转移性#
48
#转移性前列腺癌#
53
#PRO#
57