Advanced Science:心脏病发作后,锰增强磁共振或可提高患者生存率
2021-05-12 MedSci原创 MedSci原创
据英国心脏基金会称,心脏病和循环系统疾病占英国所有死亡人数的四分之一,相当于每年超过160,000例死亡,也就是说每三分钟就有1例死于心脏病或循环系统疾病。
据英国心脏基金会称,心脏病和循环系统疾病占英国所有死亡人数的四分之一,相当于每年超过160,000例死亡,也就是说每三分钟就有1例死于心脏病或循环系统疾病。

pixabay
近日,发表在Advanced Science杂志的一项研究显示,与传统的MRI方法相比,注入微量矿物质锰(Mn2+)可以增强MRI扫描,以提供更精准的的心脏成像。如果在心脏病发作的最初几个小时内进行锰增强MRI检查,则可用于确定单个患者的最佳治疗方案,有助于调节心肌变化,从而进一步提高生存机会。这一发现若在人类机体中得到证实,或会对心脏病诊疗产生重大影响。
该研究在小鼠模型中进行实验,评估微量矿物质锰对心肌细胞跳动率和电生理的影响。研究人员通过在三个关键间隔检查梗死面积和血供来评估发现:在诱发心肌梗死后的1小时,1天和14天。
结果显示,锰增强MRI提供了一种重要的新方法,可用于评估MI后1小时内的心肌生存能力。高剂量的锰离子可减少钙离子的心肌收缩力,但不会改变动作电位。补充CaG可以减少这些影响,从而支持在基于锰离子的MRI造影剂中使用CaG 。
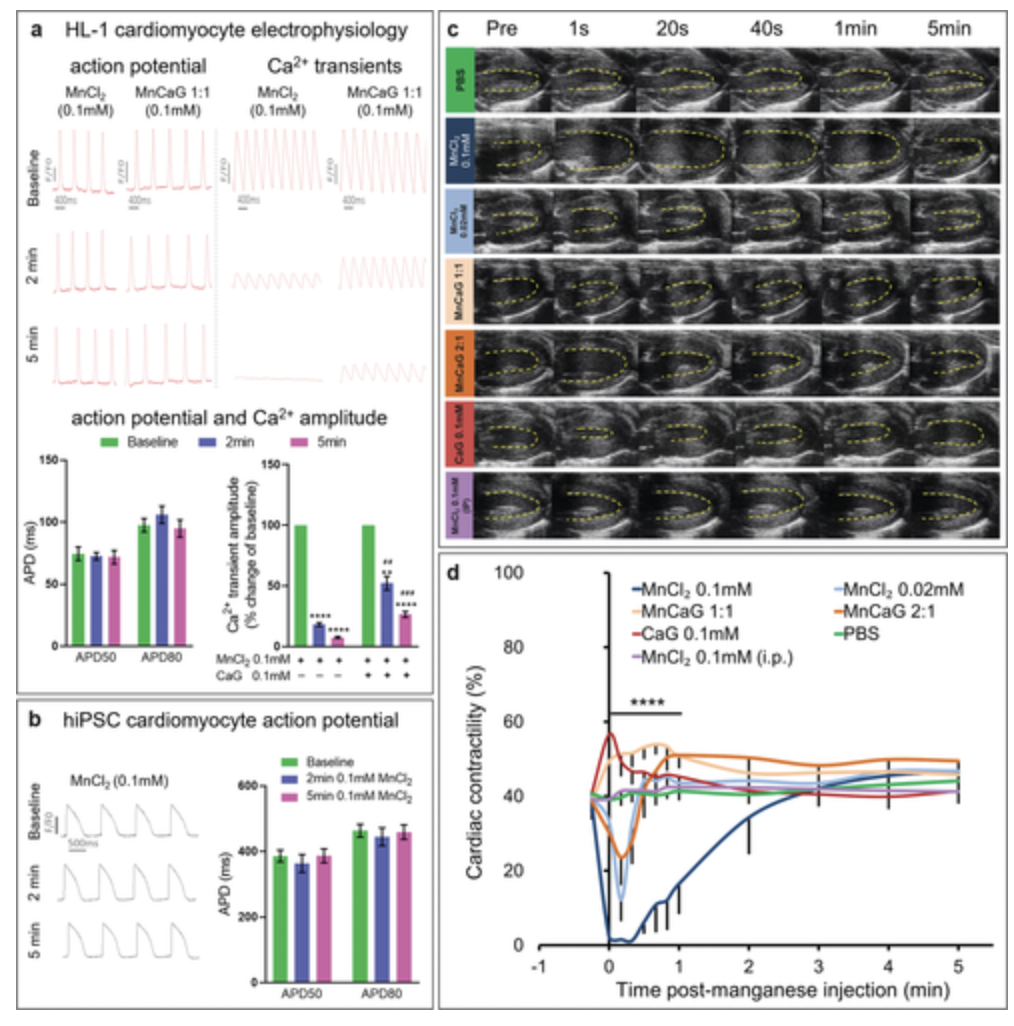
锰对心脏电生理和功能的影响.
结果进一步显示,定量T1映射锰增强MRI(MEMRI)显示活细胞中缺血性损伤(反映增加的Mn 2+摄取)后R1急剧增加,表明MEMRI可用于优化调节钙离子,进而干预心肌梗塞后体内的稳态。此外,MEMRI比LGE-MRI更早地量化梗死面积,并在不可逆细胞死亡发生之前提供早期测量方法。这种方法将在针对缺血性损伤和再灌注早期事件的治疗方法的临床前评估中大量使用。
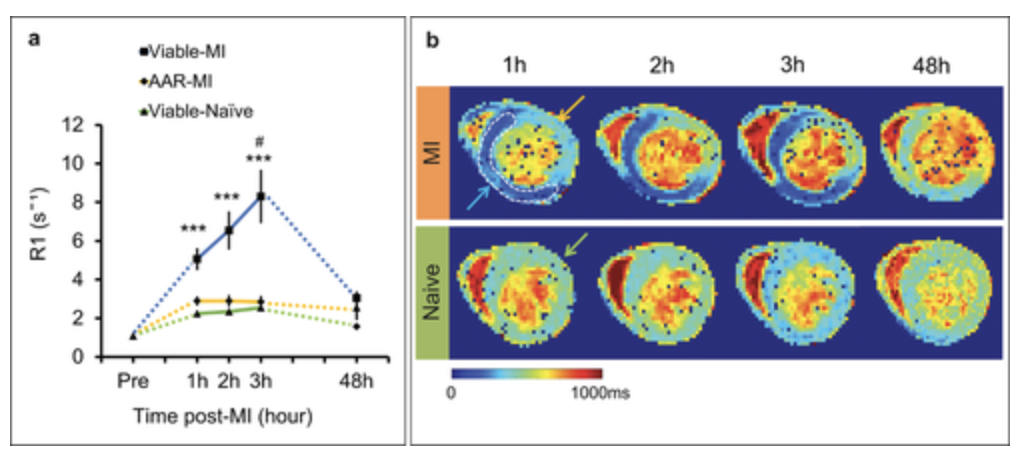
MI后急性摄取锰的T1图谱.
研究人员表示,“磁共振成像(MRI)越来越多地用于诊断有关心脏疾病的信息,MEMRI可直接评估心脏病患者发作后早期心肌生存力。”
原始出处
Nur Hayati Jasmin et al. Myocardial Viability Imaging using Manganese‐Enhanced MRI in the First Hours after Myocardial Infarction, Advanced Science (2021). DOI: 10.1002/advs.202003987
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#患者生存#
97
#Advanced#
91
#生存率#
70
#磁共振#
67
#SCIE#
81