Eur Heart J:醛固酮在慢性肾病和肾脏结局中的作用
2022-08-10 MedSci原创 MedSci原创
慢性肾病患者血清醛固酮水平升高与肾脏疾病进展风险增加独立相关,与糖尿病无关。这些结果为MR拮抗剂延缓慢性肾病进展提供了机制证据,并提示它们可能在非糖尿病患者中也有作用。
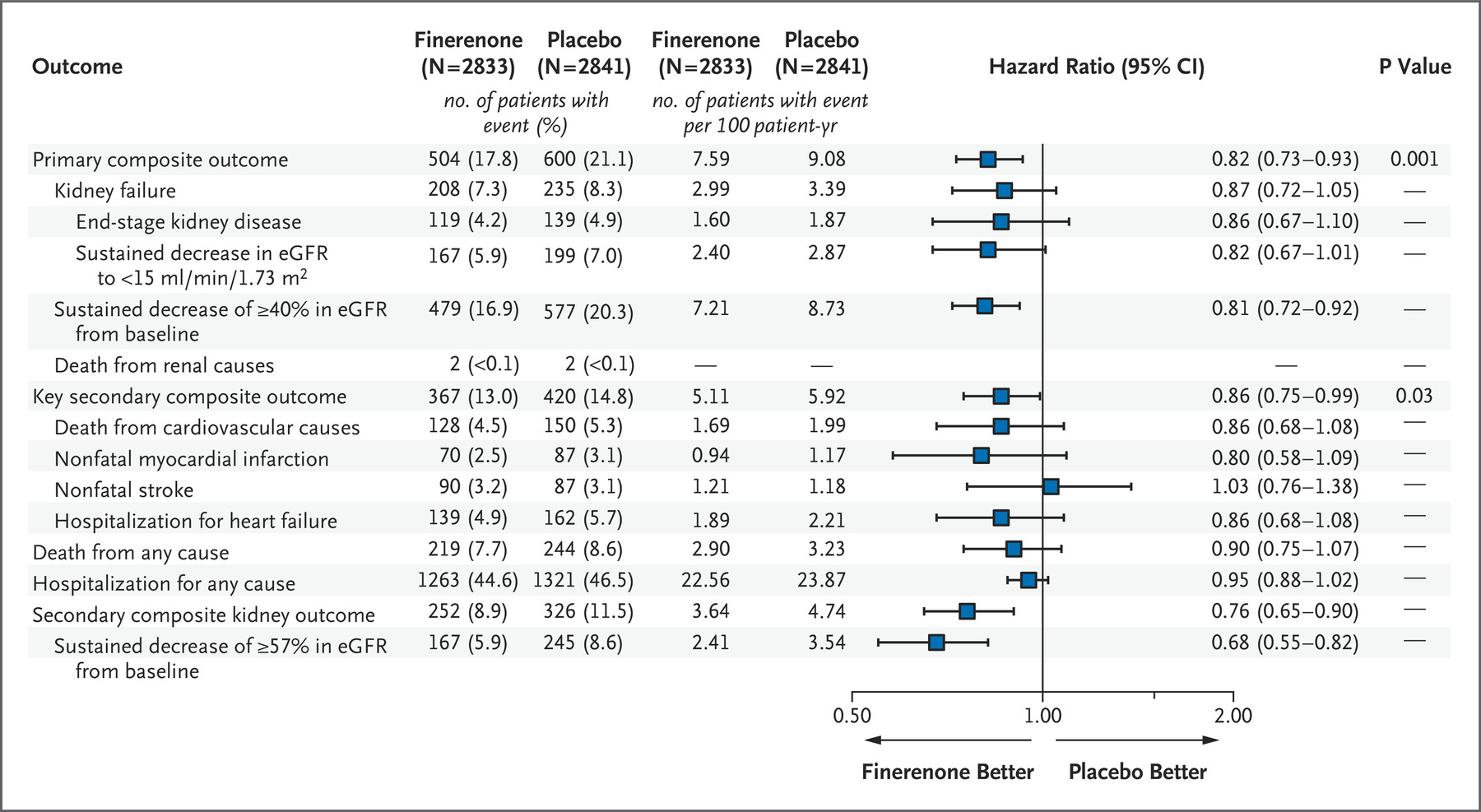
随机对照试验已经证明了盐皮质激素受体(MR)拮抗剂能够延缓糖尿病慢性肾病进展;然而,他们还没有调查醛固酮的作用,以及这些有益的效应是否可以在没有糖尿病的个体中也能观察到。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,在3680名慢性肾功能不全队列参与者中探究了血清醛固酮浓度与肾脏疾病进展之间的关系。
该研究的主要结局为慢性肾病进展[定义为估计的肾小球滤过率(eGFR)下降50%或终末期肾脏疾病(以先发生者为准)的综合结局]。研究人员使用Cox比例风险模型评估血清醛固酮与肾脏疾病预后之间的关系。
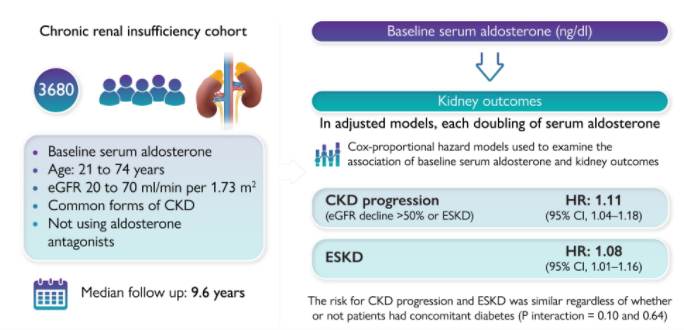
基线时,较高的醛固酮浓度与较低的表皮生长因子受体、较低的血清钾、较高的尿钾和蛋白质排泄有关。在平均9.6年的随访中,1412名参与者发生了慢性肾病进展。在调整后的模型中,血清醛固酮水平每增加一倍,慢性肾病进展风险增加11%[风险比为1.11,95%可信区间为1.04-1.18]。血清醛固酮水平最高的个体与水平最低的个体相比,慢性肾病进展风险增加45%(风险比为1.45,95%可信区间为1.22-1.73)。无论患者是否合并糖尿病,慢性肾病进展的风险是相似的(相互作用p=0.10)。
由此可见,慢性肾病患者血清醛固酮水平升高与肾脏疾病进展风险增加独立相关,与糖尿病无关。这些结果为MR拮抗剂延缓慢性肾病进展提供了机制证据,并提示它们可能在非糖尿病患者中也有作用。
原始出处:
Ashish Verma,et al.Aldosterone in chronic kidney disease and renal outcomes.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article-abstract/doi/10.1093/eurheartj/ehac352/6652163?redirectedFrom=fulltext
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












q
46
#ART#
65
#醛固酮#
58
#肾脏结局#
56
#HEART#
72