Euro Radio颈动脉易损斑块与脑小血管疾病及急性缺血性卒中的相关性
2022-08-22 shaosai MedSci原创
斑块内出血(IPH)、薄或破裂的纤维帽(FC)和不规则的斑块表面等易损斑块特征是评估缺血性卒中风险的有效指标。
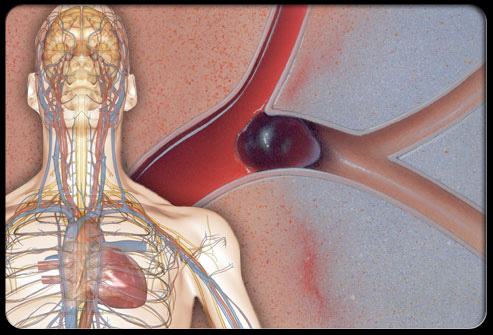
 众所周知,卒中是世界范围内导致死亡和残疾的主要原因之一,大动脉粥样硬化和小血管闭塞都可能导致急性缺血性卒中(AIS)。以往的一些研究表明,斑块内出血(IPH)、薄或破裂的纤维帽(FC)和不规则的斑块表面等易损斑块特征是评估缺血性卒中风险的有效指标。小血管闭塞是脑小血管疾病(CSVDs)的病理之一,占缺血性卒中的25%。越来越多的证据表明,白质增生(WMHs)和裂隙等由MRI确定的CSVDs与缺血性卒中的风险明显相关。虽然颈动脉粥样硬化和CSVDs是不同的血管疾病,但许多研究者发现这些疾病常在有脑血管症状的患者中并存。
众所周知,卒中是世界范围内导致死亡和残疾的主要原因之一,大动脉粥样硬化和小血管闭塞都可能导致急性缺血性卒中(AIS)。以往的一些研究表明,斑块内出血(IPH)、薄或破裂的纤维帽(FC)和不规则的斑块表面等易损斑块特征是评估缺血性卒中风险的有效指标。小血管闭塞是脑小血管疾病(CSVDs)的病理之一,占缺血性卒中的25%。越来越多的证据表明,白质增生(WMHs)和裂隙等由MRI确定的CSVDs与缺血性卒中的风险明显相关。虽然颈动脉粥样硬化和CSVDs是不同的血管疾病,但许多研究者发现这些疾病常在有脑血管症状的患者中并存。
有研究证明,大动脉粥样硬化狭窄患者的CSVDs与脑血管事件之间存在关联。然而,目前还不清楚与CSVDs共存的颈动脉粥样硬化的易损斑块特征是否比单独的斑块特征与AIS有更强的关联。
近日,发表European Radiology杂志的一项研究探讨了与CSVDs共存的颈动脉易损斑块特征与AIS风险之间的关系,并进一步确定了共存的疾病与AIS的关系是否比单一疾病更加密切,为临床进一步阐明两种疾病的病理生理及进展因素提供了参考依据。
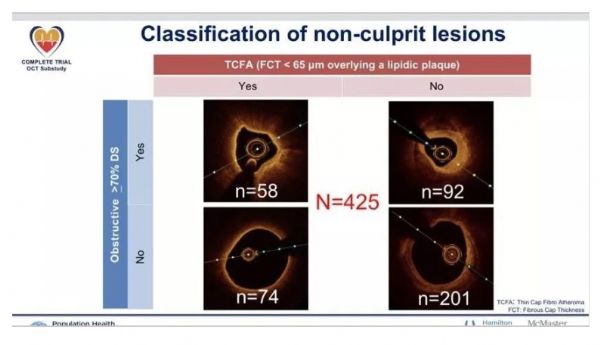
本研究招募了同时患有脑血管症状和颈动脉斑块的患者进入研究。该人群被分为两组(AIS和短暂性缺血性卒中(TIA))。评估了颈动脉斑块(包括管腔狭窄和斑块易损性)和CSVDs(如白质增生(WMHs)和裂隙)的MRI特征。并存的疾病被定义为至少存在一个颈动脉斑块特征和一个或多个CSVDs特征。进行多变量逻辑回归,研究共存疾病和AIS之间的关联。
在招募的634名患者中(平均年龄:59.1±11.3岁;429名男性),312名(49.2%)患者患有AIS。与TIA患者相比,这些受试者的颈动脉易损斑块、裂隙和中重度WMH(Fazekas总分3-6分)的发生率更高(分别为42.6% vs. 29.5%,59.6% vs. 26.4%,69.9% vs. 60.6%,所有P<0.05)。多变量分析显示,与单独的颈动脉病变相比,颈动脉斑块特征与裂隙或中重度WMHs共存与AIS有更强的关联(均为P<0.05)(即易损斑块与裂隙共存与单独的易损斑块,调整后的几率比:3.67 vs. 1.62)。
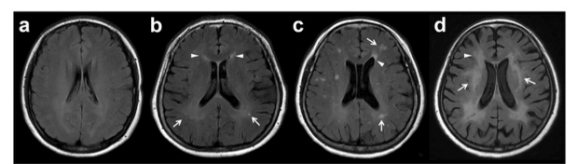
图 a(Fazekas总分:0),脑室周围或深部白质没有观察到高信号。 b(Fazekas总分:2),深部白质的点状高信号(白色箭头)(Fazekas评分:1)和脑室周围的帽状高信号(白色箭头)(Fazekas评分:1)。c(Fazekas总分:3),可以看到深层白质高信号(Fazekas评分:2)和脑室周围的帽状高信号(Fazekas评分:1,白色箭头)开始汇合。 d(Fazekas总分:6),脑室周围病变(白色箭头)延伸到深层白质(Fazekas评分:3),深层白质中出现大量病变(白色箭头)汇合(Fazekas评分:3)
本研究发现,与单独的颈动脉疾病相比,颈动脉易损斑块及脑小血管疾病与急性缺血性卒中有更强的关联。本研究结果表明,全面评估颈动脉斑块的易损性和脑小血管疾病有助于更好地对缺血性卒中进行风险分层。
原文出处:
Jin Li,Hengqu Wu,Hailun Hang,et al.Carotid vulnerable plaque coexisting with cerebral small vessel disease and acute ischemic stroke: a Chinese Atherosclerosis Risk Evaluation study.DOI:10.1007/s00330-022-08757-9
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#缺血性#
55
#相关性#
72
#缺血性卒#
65
#小血管疾病#
74
#PE#
85
#颈动脉#
77
#斑块#
0
#脑小血管疾病#
53
#血管疾病#
80