急性胸痛,警惕这10大疾病作祟!
2016-09-21 侣行家 医学界心血管频道
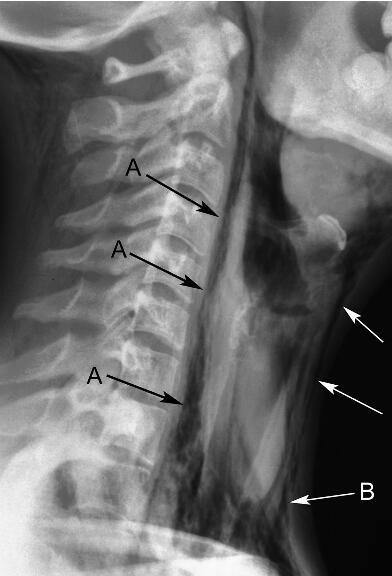
胸痛是心内科临床常见的主诉之一,由于鉴别诊断难度较大,常存在误诊、漏诊的可能性,因此需要充分重视。体检一般的体格检查,如脉搏、血压、呼吸、体温可以帮助评估患者的一般情况, 判断循环或呼吸衰竭等短期内威胁生命的并发症,指导用药,纠正生命体征和避免危险因素的发展。此外,胸腹部的体格检查包括视、触、叩、听以及各类辅助检查对胸痛的鉴别也会起到一定帮助。1.心绞痛或心肌梗死[1]出冷汗提示心绞痛或AMI
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













这几个总结的好
84
以前一直以为夹层血压会降低
107
重视胸痛
79
不典型的患者最可怕了,要特别小心
83
继续关注
93
666845472805
0
学习起来
43
继续学习
42
继续关注
42