Neuropathol. Appl. Neurobiol:癫痫患者脑皮质变薄与小胶质细胞激活有关
2021-11-10 自由影像之光 MedSci原创
在常见的人类癫痫病中,大脑皮层厚度明显减少在神经影像学上可检测到,并具有重要的临床后果,但其原因尚不清楚。
在常见的人类癫痫病中,大脑皮层厚度明显减少在神经影像学上可检测到,并具有重要的临床后果,但其原因尚不清楚。
Sanjay M. Sisodiya等使用系统级分析研究了皮质变薄的潜在机制。采用细胞型反褶积、差异表达分析和细胞型富集分析来鉴别细胞型分布的差异。使用Iba1免疫标记技术对癫痫患者的死后脑组织进行了跟踪研究。此外,为了研究皮质变薄的因果效应,在获得性癫痫小鼠模型中使用了细胞类型特异性耗竭。
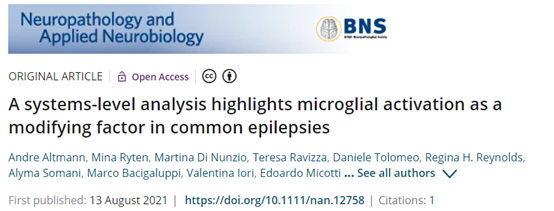
分析流程
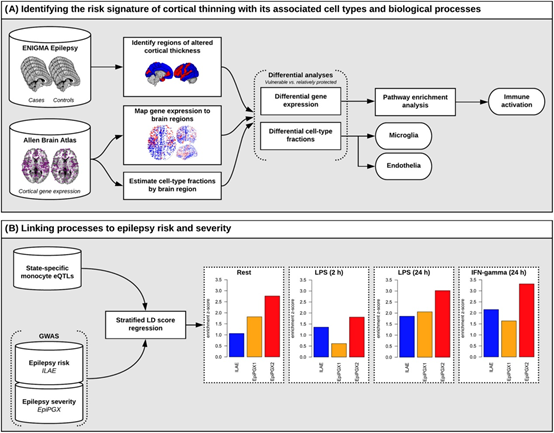
癫痫患者死后脑组织中存在过度激活的小胶质细胞。
该研究在皮质厚度减少的区域发现了小胶质细胞和内皮细胞的升高。差异表达的基因显示了小胶质标记的富集,特别是激活的小胶质状态。癫痫患者的尸检脑组织分析证实小胶质细胞过度激活。

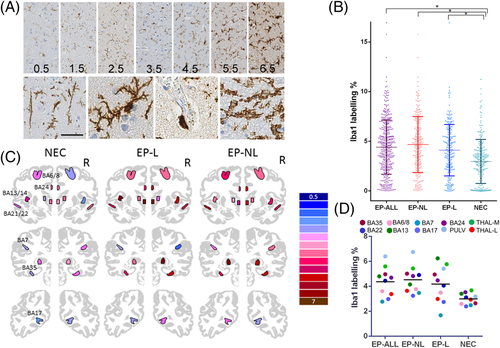
疾病早期小胶质细胞缺失对癫痫小鼠内嗅皮层厚度、神经元细胞缺失和认知缺陷的影响
在小鼠模型中,在疾病发展的早期,激活的小胶质细胞的短暂耗竭阻止了颞叶皮层的变薄和神经元细胞的丢失。尽管慢性癫痫发作的发展没有受到影响,但在非空间记忆测试中,小胶质细胞早期缺失的癫痫小鼠并没有出现缺陷。
这些汇聚的数据强烈暗示了皮质变薄区存在激活的小胶质细胞,代表了关注和疾病改变的新维度可能不同于癫痫控制。
该研究指出了神经炎症通路和潜在的特定分子的重要作用,如IFN-γ。然而,小胶质细胞状态和功能的多样性,以及神经元、星形胶质细胞和小胶质细胞之间复杂、动态的相互作用,至少可以促进癫痫发生。该研究对小胶质细胞激活在不同类型癫痫中的广泛作用的关键观察,将其转化为预防脑物质不可逆损失的治疗方案需要定义不同类型癫痫中变薄的时间进程。还需要开发安全、有效和可耐受的治疗方法,以精确的机制为目标,而不影响对脑组织的免疫监测,这是对各种神经疾病的需要。
原文出处
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#Pathol#
69
#Bio#
59
#Biol#
67
#脑皮质#
56
#癫痫患者#
60
#胶质细胞#
72
🐮
78