Seminars in Cancer Biology:肠道微生物有助于抗癌免疫调节
2021-03-20 MedSci原创 MedSci原创
肠道微生物区系在影响肿瘤发生和癌细胞对治疗药物的反应方面具有重要作用。微生物区系对癌症的显著影响推动了操纵微生物区系来预防和治疗癌症的努力。微生物操作可以作为传统癌症治疗的辅助手段。
微生物区系影响人类健康和多种疾病的发展,包括癌症。微生物可以通过积极或消极的方式影响肿瘤的发生和发展。此外,肠道微生物区系的组成影响癌症治疗药物的疗效和毒性以及治疗耐药性。微生物区系对肿瘤发生和癌症治疗的显著影响提供了令人信服的证据,支持操纵微生物网络是治疗和预防癌症的一种有前途的战略。特定的微生物或微生物生态系统可以通过多种过程进行修饰,治疗方法和途径也在不断发展。微生物操作可以作为传统癌症治疗(如化疗和免疫治疗)的辅助手段。此外,在标准治疗失败后,这种方法显示出作为一种独立治疗的巨大前景。此外,这样的策略还可以避免出现导致停止治疗的毒副作用,从而使患者受益。更好地了解癌症患者的宿主-微生物生态系统,以及开发操纵微生物群的方法,将有助于扩大精确癌症治疗的前沿,从而改善患者护理。Kentaro Inamura在Seminars in Cancer Biology杂志发表综述讨论了微生物区系在肿瘤发生和癌症治疗中的作用,重点讨论了利用微生物区系来抗击癌症的努力。
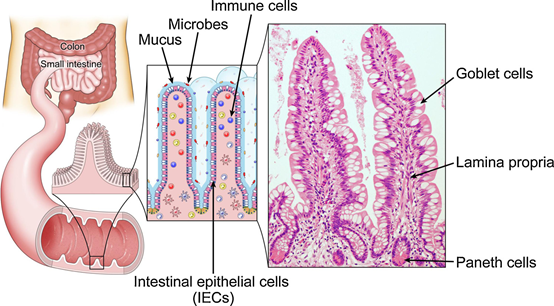
肠道、细胞和微生物的结构。肠粘膜由单层肠上皮细胞(IECS)组成,包括杯状细胞和潘氏细胞,以及下层固有层。杯状细胞会产生一层粘液层,阻碍微生物与IECS的结合。潘氏细胞通过释放抗菌肽来阻止微生物入侵。IECS下的固有层含有多种类型的免疫细胞,包括抗原提呈细胞(如树突状细胞)、T细胞和B细胞。
1.通过宿主-微生物区系相互作用的免疫调节微生物区系
肠道微生物区系通过调节局部和系统的免疫反应来塑造宿主的免疫系统。肠粘膜是肠壁的内室,由几种类型的肠上皮细胞(IECS)组成,包括杯状细胞和潘氏细胞,以及下面的固有层
高脚杯细胞产生一层粘液层,通过空间位阻阻碍微生物与IECS的结合,并作为微生物粘附的可释放诱饵。相反,微生物是产生粘液的先决条件,无菌(GF)小鼠的粘液层缺失就说明了这一点。此外,Paneth细胞通过释放抗菌肽来阻止微生物入侵,这些抗菌肽维持内粘液层的无菌状态。IECS下的固有层含有多种免疫细胞,包括抗原提呈细胞(如树突状细胞)、T细胞和B细胞。
微生物通过与表达模式识别受体(PRRs)(例如,Tolllike受体[TLRs])的免疫细胞相互作用来触发局部免疫反应。微生物或微生物衍生的元素(如成分、产品、代谢物)通过与PRRs的相互作用激活树突状细胞。这些遭遇导致被激活的树突状细胞从胃肠道移动到肠系膜淋巴结(MLN),在那里它们呈递微生物衍生的抗原,随后诱导幼稚T细胞分化为效应性T细胞,特别是调节性T细胞(Tregs)和辅助性T细胞(Th17)。这些效应器T细胞的一部分会迁移回胃肠道,并影响局部免疫反应。剩下的进入体循环,影响系统免疫。Treg通过释放抗炎细胞因子(如IL-10、转化生长因子-β)或树突状细胞的参与,介导免疫系统从促炎状态转变为抗炎状态[41]。相反,Th17细胞通过分泌免疫刺激细胞因子(如IL-17)或通过激活和招募中性粒细胞来介导免疫系统向促炎状态的转变。GF小鼠的固有层缺乏这些促炎的Th17细胞;然而,它们的生成是由一种特殊的细菌亚群恢复的,这种亚群被称为节段性丝状细菌。这一耐人寻味的关系强烈表明微生物在Th17细胞激活中的重要作用。
2.微生物对癌症发生和发展的影响
微生物以组织特异性的方式促进或抑制肿瘤。一些微生物通过产生有毒或致瘤产物直接促进肿瘤的发生和发展,并通过创造促炎或抗炎的微环境间接促进肿瘤的发生和发展。相反,其他微生物通过增强宿主的抗肿瘤免疫反应,在胃肠道或其他器官发挥肿瘤抑制作用。特定的微生物衍生产品(如短链脂肪酸)创造了抑制肿瘤的微环境。例如,微生物衍生的SCFA丁酸盐分子通过微生物发酵纤维在肠道中释放,通过灭活肿瘤细胞中的组蛋白去乙酰化酶和通过将免疫系统转变为抗炎状态来抑制肿瘤生长。
3.微生物区系对化疗疗效和毒性的影响
化疗药物的作用与宿主的免疫反应密切相关。微生物群的组成影响着这一反应,不可避免地影响化疗的疗效、毒性以及化疗耐药性。某些细菌需要化疗才能发挥其抗肿瘤作用,而另一些细菌则会产生抗药性。同样,特定的细菌会引起或抑制化疗引起的不良反应。
微生物区系通过多种机制调节化疗效果和毒性,这些机制统称为TIMER机制框架(转位、免疫调节、代谢、酶降解、多样性降低)。当化疗药物破坏肠道屏障时,细菌会从肠道转移到次级淋巴器官(如淋巴细胞、脾脏)。反过来,胃肠道微生物通过免疫调节影响化疗的疗效和毒性。例如,环磷酰胺(CTX)增加肠道通透性,并诱导某些肠道微生物移位到MLN和脾脏,在那里它们通过调节局部和系统免疫来刺激CTX的抗肿瘤活性。胃肠道微生物可能直接决定化疗药物的药理命运,从而决定化疗药物的益处和副作用。事实上,一项高通量研究系统地确定了一系列药物代谢微生物酶。这些微生物特有的酶直接影响肠道和全身的药物代谢,并解释肠道微生物的药物代谢作用。作为微生物通过酶降解产生的影响的一个例子,猪鼻支原体使吉西他滨脱氨基以减少其有益作用。此外,某些化疗药物会降低微生物多样性,从而产生不良影响。
4.微生物区系对免疫治疗效果和毒性的影响
癌细胞在宿主体内存活的能力是通过产生免疫抑制微环境来实现的。增强宿主抗癌免疫的有益效果为制定有效的免疫治疗策略提供了重要信息。这种方法极大地改变了恶性肿瘤的治疗格局,特别是当它利用免疫检查点阻断的时候。不幸的是,williamhill asia 缺乏准确预测免疫疗法临床反应的生物标记物,williamhill asia 对决定其疗效和毒性的机制的了解不足,显然必须扩大。新的证据表明,微生物区系通过调节宿主的局部和系统免疫反应来影响免疫治疗的反应。因此,利用微生物、它们的成分,或两者兼而有之,可能有助于识别可能有助于癌症免疫疗法发展的生物标记物和治疗靶点。
5.微生物干预作为癌症治疗方法
微生物区系对肿瘤发生和癌症治疗的显著影响提供了令人信服的证据,表明操纵微生物网络是治疗癌症的一种很有前途的策略。特定的微生物或微生物生态系统可以通过许多过程进行修饰,治疗方法和途径正在迅速演变。
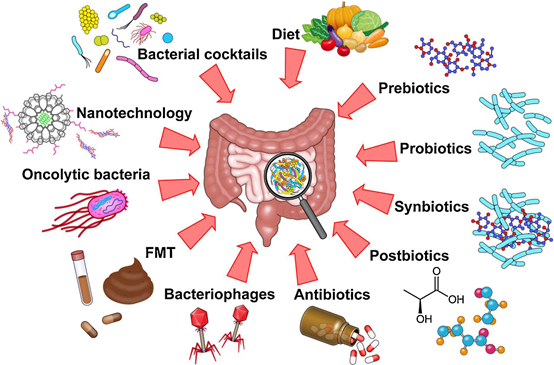
越来越多的证据表明,肠道微生物区系在影响肿瘤发生和癌细胞对治疗药物的反应方面具有重要作用。微生物区系对癌症的显著影响推动了操纵微生物区系来预防和治疗癌症的努力。微生物操作可以作为传统癌症治疗的辅助手段,也可以作为标准治疗失败后的独立治疗。对于这些有希望的策略的应用,还需要在描绘复杂的微生物网络方面做出更大的努力。关于微生物的全部范围和每种微生物在特定癌症类型中的特定功能的知识仍然有限。在与微生物区系相关的研究中,研究人员必须认识到,小鼠模型可能不能精确地模拟人类宿主-微生物区系生态系统。例如,实验室小鼠的肠道微生物区系明显不同于其野生小鼠的肠道微生物区系。在实验室小鼠中重建野生小鼠的微生物区系可以恢复对肿瘤形成的保护,这突显了野生和实验室微生物区系之间的功能差异。此外,移植到小鼠体内的肿瘤细胞不会经历多步骤的肿瘤发生,也不会与微环境密切相互作用。此外,肿瘤移植程序可以改变肿瘤特性和抗肿瘤免疫,人和鼠微生物区系之间的组成差异明显地混淆了结果。因此,应该努力开发一种真实模仿人类宿主-微生物区系生态系统的模型。此外,在某些特定环境中高度丰富的微生物在功能上不一定重要。相反,具有实验证明功能的特定微生物应该成为癌症治疗学的靶标。为了深入了解复杂的宿主-微生物区系相互作用,结合了微生物学、分子病理学和流行病学的分子病理流行病学(MPE)方法,由于其多层次和多维度的设计,可能是很有前途的。不断增加的关于癌症宿主-微生物生态系统的知识,加上不断发展的方法学,将有助于扩大精确癌症治疗的前沿,以改善患者护理。
原文出处
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










肠道微生物研究
68
#cancer biology#
72
#Bio#
80
#Biol#
58
#微生物#
67
重大利好
102
确实是很有前途的分析
103