【一般资料】
患者男,56岁
【既往史】
【主诉】
本次因“胸椎管狭窄”入院。
【辅助检查】
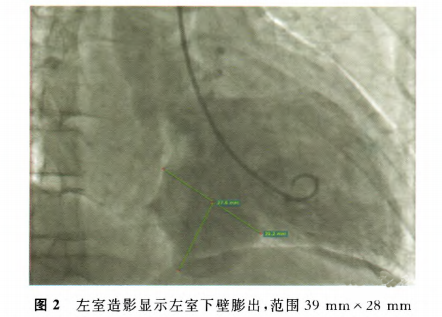
术前常规心脏超声检查发现左室下壁基底段心肌变薄,向外膨出约40mm×30mm(图1),部分切面可见附壁低回声,且该处心肌似与左室心肌呈同步运动,彩色多普勒未见明显血流出入该膨出的腔室,因受检时无明确的冠状动脉狭窄病史,提示该膨出部分为左室憩室可能。心电图示QT间期延长,T波改变。冠状动脉造影提示冠心病,多支病变,左前降支近段中重度狭窄,左旋支远端全闭,右冠状动脉近段全闭。左室造影可见左室下壁向外膨出部分显影,约39mm×28mm(图2),大小随心动周期无明显变化。

【治疗经过】
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#血管病#
26
#超声表现#
41
学习了感谢分享
68
学习了感谢分享
54
#血管病变#
40
#左心室#
28
#憩室#
34
学习了.谢谢分享
66
厉害了我的哥
61